When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. But how do regulators know it’s truly the same? The answer lies in the 80-125% rule-a quiet but powerful standard that decides whether a generic drug can hit the market. This isn’t about how much active ingredient is in the tablet. It’s not about price. It’s about what happens inside your body after you swallow it.
What the 80-125% Rule Actually Means
Many people think the 80-125% rule means generic drugs can contain anywhere from 80% to 125% of the active ingredient compared to the brand. That’s wrong. The rule doesn’t control the amount of drug in the pill. It controls how your body absorbs it. Here’s the real definition: For two drugs to be considered bioequivalent, the 90% confidence interval of the ratio of their geometric means for two key measurements-AUC and Cmax-must fall entirely between 80% and 125%. AUC stands for Area Under the Curve, which tells you how much of the drug your body is exposed to over time. Cmax is the highest concentration the drug reaches in your bloodstream. Both are measured after a single dose in healthy volunteers. These numbers come from statistical analysis of data collected in clinical studies. The data is log-transformed because drug concentrations don’t follow a normal bell curve-they follow a log-normal distribution. On a logarithmic scale, 80% and 125% are symmetric around 100%, making the math work cleanly. That’s why regulators use this range instead of a simple ±20%.Why 90% Confidence Interval? Not 95%
You’ve probably heard of 95% confidence intervals in science. But for bioequivalence, it’s 90%. Why? Because regulators are okay with a 10% total risk of error-5% on the low side and 5% on the high side. That’s a deliberate trade-off. If they used 95%, they’d need way more people in the study, making it slower and more expensive. The 90% interval strikes a balance between scientific rigor and practicality. The rule doesn’t say the average difference must be zero. It says the entire range of likely values must stay within 80-125%. Even if the average ratio is 95%, if the confidence interval stretches from 75% to 105%, the drug fails. That’s because 75% is outside the allowed range. The rule is strict: no part of the interval can leak out.Who Uses This Rule? Everyone.
The 80-125% rule isn’t just an American standard. It’s global. The U.S. FDA, the European Medicines Agency (EMA), the World Health Organization (WHO), Health Canada, China’s NMPA-they all use nearly identical criteria. This harmonization means a generic drug approved in one country has a much easier path to approval in another. It’s why the global generic drug market is worth over $227 billion. This uniformity didn’t happen by accident. It came from decades of scientific debate. In the 1980s, regulators realized the old ±20% additive rule didn’t work well for pharmacokinetic data. The multiplicative 80-125% rule replaced it because it better reflected how drug exposure changes proportionally-not linearly. By 1992, the FDA formally adopted it. Other agencies followed, and today, it’s the gold standard.
When the Rule Doesn’t Apply
The 80-125% rule works well for most drugs. But not all. Some drugs need tighter limits. For example, drugs with a narrow therapeutic index-like warfarin, levothyroxine, or phenytoin-can cause serious harm if blood levels shift even slightly. For these, regulators sometimes require a 90-111% range. The FDA issued draft guidance in 2022 specifically for these drugs. On the other end, highly variable drugs-where people’s bodies absorb the drug very differently from one another-also need special treatment. If a drug’s within-subject coefficient of variation is above 30%, the standard 80-125% range might be too strict. That’s where scaled average bioequivalence (SABE) comes in. Under SABE, the acceptance range can widen-up to 69.84-143.19% for Cmax-based on how variable the reference drug is. The EMA has used this since 2010. The FDA started allowing it in 2021 for certain products.What Happens in a Bioequivalence Study?
To prove bioequivalence, companies run crossover studies. Typically, 24 to 36 healthy volunteers take both the generic and brand-name drug, in random order, with a washout period in between. Blood samples are taken over 24 to 72 hours. The data is analyzed using statistical software that calculates the geometric mean ratio and its 90% confidence interval. The study must show both AUC and Cmax meet the 80-125% rule. One failing means the whole thing fails. Even if AUC passes but Cmax is just barely outside-say, 126%-the generic is rejected. This isn’t arbitrary. Cmax affects how fast the drug works. AUC affects how long it lasts. Both matter. For complex drugs-like extended-release pills, inhalers, or topical creams-the process gets harder. The FDA launched its Complex Generics Initiative in 2018 to tackle these. Some complex products now require special dissolution testing instead of full human studies, thanks to the 2021 Bioequivalence Waiver Program.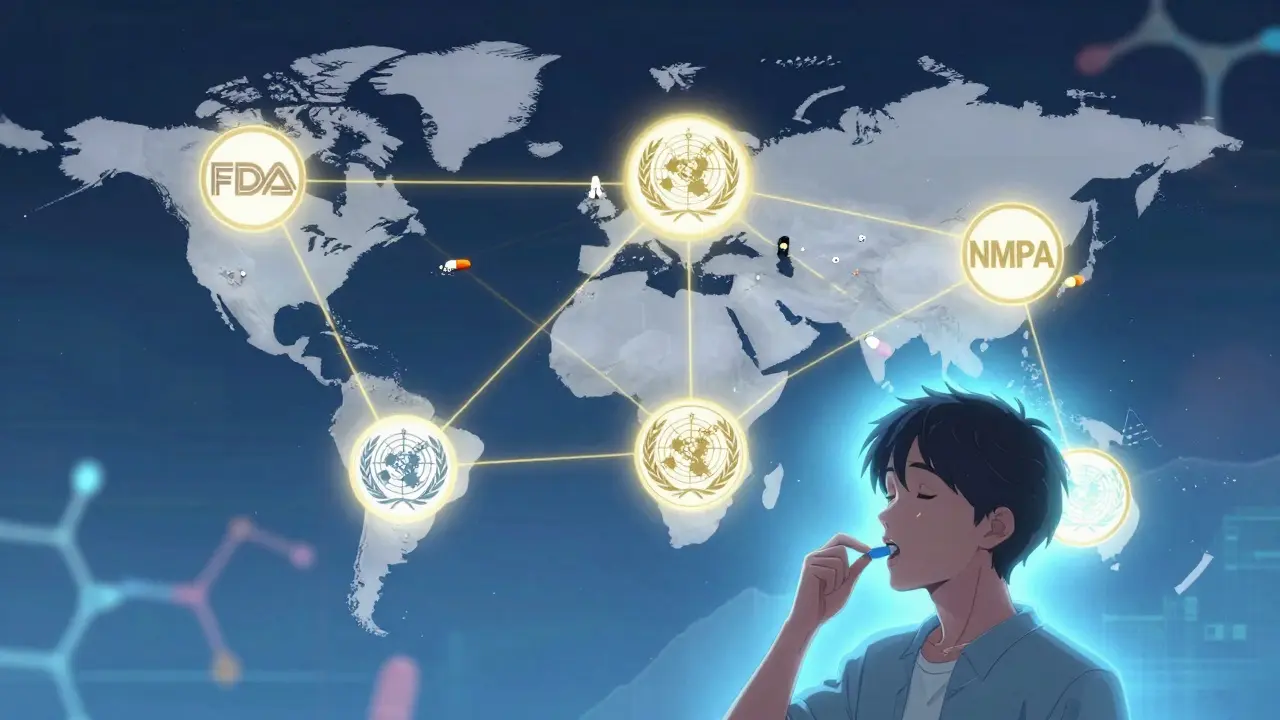
Myths and Misunderstandings
There’s a lot of confusion out there. A 2022 survey found 63% of pharmacists believed the 80-125% rule meant generics could contain 80-125% of the active ingredient. That’s not true. In reality, most generics contain 95-105% of the labeled amount-the same as brand drugs. The rule is about absorption, not composition. Patients worry too. Online forums are full of people afraid their generic seizure medication won’t work. But real-world data tells a different story. Between 2003 and 2016, the FDA approved over 2,000 generic drugs. Only 0.34% needed label changes due to bioequivalence issues after launch. Most problems reported by patients-like nausea or dizziness-are linked to inactive ingredients, not the active drug. A 2022 survey of 412 neurologists found that 28% had seen occasional issues with generic anti-seizure drugs. But only 4% thought it was because of bioequivalence standards. The rest pointed to formulation differences-fillers, coatings, or manufacturing changes-that affect how the pill dissolves in the gut.What’s Next for the 80-125% Rule?
The rule has held up for nearly 40 years. But science is evolving. Researchers are now exploring model-informed bioequivalence-using computer simulations to predict how a drug behaves based on its chemical structure and previous data. This could reduce the need for human trials in the future. The FDA’s 2023-2027 Strategic Plan includes $15 million for modernizing bioequivalence tools. The International Pharmaceutical Regulators Programme is working on guidelines for complex generics, with updates expected by late 2024. And with pharmacogenomics advancing, we may one day see bioequivalence standards that account for genetic differences in drug metabolism. But for now, the 80-125% rule remains the backbone of generic drug approval. It’s not perfect. It’s not based on clinical trials proving identical outcomes. It’s based on decades of pharmacokinetic data and expert judgment. And yet, it works. Over 90% of prescriptions in the U.S. are filled with generics. Millions of people take them every day without issue. That’s the real test.What You Should Know as a Patient
If you’re switching from brand to generic, you don’t need to worry about the 80-125% rule. It’s already been checked. The FDA and other agencies don’t approve drugs that might cause harm. If your doctor or pharmacist tells you the generic is equivalent, they’re right. If you notice a change in how you feel after switching-like new side effects or reduced effectiveness-don’t assume it’s the bioequivalence rule. Talk to your doctor. It could be a change in fillers, coatings, or even your body’s response to a different manufacturing batch. But it’s almost never because the active ingredient is too weak or too strong. The 80-125% rule isn’t about cutting corners. It’s about making safe, affordable medicine accessible to everyone. And so far, it’s done exactly that.Is the 80-125% rule the same as saying generics are 80% as strong as brand drugs?
No. The 80-125% rule does not refer to the amount of active ingredient in the pill. It refers to the 90% confidence interval of the ratio of pharmacokinetic measurements-AUC and Cmax-between the generic and brand drug. Generic drugs typically contain 95-105% of the labeled active ingredient, just like brand drugs. The rule ensures your body absorbs the drug at a similar rate and extent, not that the pill contains less medicine.
Why is a 90% confidence interval used instead of a 95% one?
A 90% confidence interval allows for a 10% total risk of error-5% on each end-while keeping studies practical. Using a 95% interval would require much larger sample sizes, making studies more expensive and slower. Regulators chose 90% as a balance between scientific certainty and feasibility. The 80-125% range already accounts for acceptable variation in drug absorption, so a 90% CI is sufficient to ensure safety.
Do all countries use the 80-125% rule?
Yes. Major regulatory agencies worldwide-including the U.S. FDA, European Medicines Agency (EMA), World Health Organization (WHO), Health Canada, and China’s NMPA-use the same 90% confidence interval of 80-125% for AUC and Cmax. This global alignment makes it easier for generic drug manufacturers to develop products for multiple markets without redesigning studies for each country.
Are there exceptions to the 80-125% rule?
Yes. For drugs with a narrow therapeutic index-like warfarin or levothyroxine-tighter limits of 90-111% may be required. For highly variable drugs (with within-subject CV >30%), regulators allow scaled average bioequivalence (SABE), which can expand the range up to 69.84-143.19% for Cmax. These exceptions are based on the drug’s behavior, not a one-size-fits-all approach.
Why do some people say generics don’t work as well?
Most complaints about generics not working are due to differences in inactive ingredients-not the active drug. Fillers, coatings, or manufacturing changes can affect how quickly the pill dissolves in the stomach. This can cause temporary side effects or changes in absorption, especially for drugs like anti-seizure medications. But these issues are not caused by the 80-125% rule. Post-market surveillance shows that less than 0.5% of approved generics require label changes due to bioequivalence concerns.