Switching to generic medications isn’t just a smart move-it’s one of the most reliable ways to cut prescription costs without sacrificing effectiveness. If you’re paying hundreds a month for maintenance drugs like blood pressure pills, cholesterol meds, or thyroid medication, you’re likely overpaying. The truth is simple: generic medications work the same as brand-name drugs, but cost up to 90% less. And this isn’t theory-it’s backed by data, real patient stories, and decades of regulatory oversight.
What Exactly Are Generic Medications?
A generic medication contains the exact same active ingredient as its brand-name version. That means if you take lisinopril for high blood pressure, it’s chemically identical to Zestril. The same goes for metformin versus Glucophage, or atorvastatin versus Lipitor. The FDA doesn’t allow generics to be sold unless they match the brand in strength, dosage, how fast they enter your bloodstream, and how well they work. This isn’t a guess-it’s a legal requirement.
What’s different? Just the filler ingredients, color, shape, or packaging. A generic pill might be white and oval instead of blue and capsule-shaped. It might say “Lisinopril 10mg” instead of “Zestril.” But the part that actually treats your condition? Identical. The FDA inspects manufacturing plants for generics just as strictly as those making brand-name drugs. There’s no corner-cutting when it comes to safety.
How Much Money Can You Really Save?
The numbers don’t lie. According to the U.S. Food and Drug Administration, generic drugs cost, on average, 85% less than brand-name versions. Over the last decade, this has saved U.S. patients more than $2.2 trillion. That’s not a typo. Trillion.
Take real examples from 2022:
- A medication that used to cost $47 per dose dropped to under $2-cutting a 30-day supply from $1,400 to under $60.
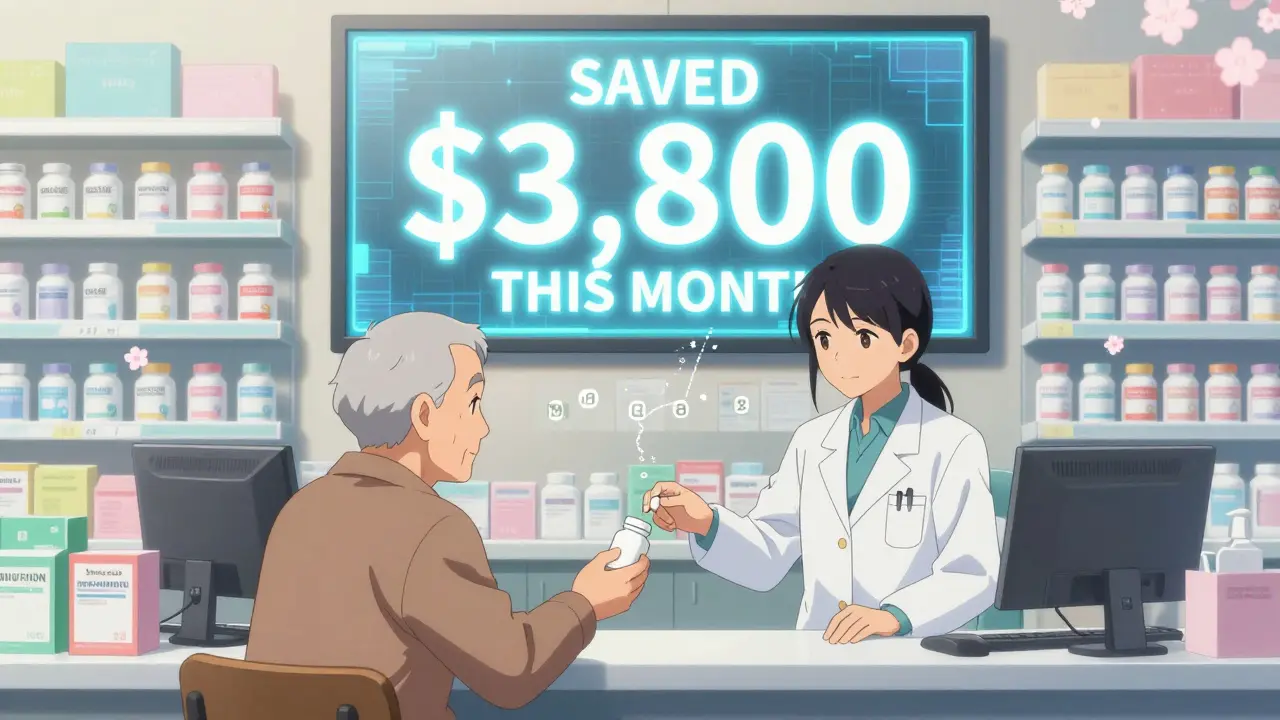
- Another drug fell from $88 per mL to less than $10 per mL, slashing monthly costs from $3,800 to $500.
These aren’t outliers. They’re routine. In 2022 alone, the FDA approved dozens of new generic drugs, each triggering massive price drops. For Medicare beneficiaries, 90% of the top 184 most-prescribed generics could be bought at Costco for under $20 for a 30-day supply. That’s cheaper than many insurance copays.
Even with insurance, switching to generics can cut your out-of-pocket costs in half. Between 2010 and 2020, the average amount patients paid directly for generic prescriptions dropped by nearly 50%. Total costs-including what insurers paid-fell by almost 80%.
Why Do Generics Cost So Much Less?
Brand-name drugs spend years and hundreds of millions of dollars on clinical trials to prove they’re safe and effective. Once approved, they get a patent that blocks competitors for 10-20 years. When that patent expires, other companies can make the same drug. They don’t need to repeat the expensive trials. They just have to prove their version delivers the same amount of active ingredient into your bloodstream at the same rate. That’s called bioequivalence-and it’s a much cheaper process.
That’s why over 100 companies now compete to make generics. More competition means lower prices. The FDA approves hundreds of new generics every year, and each one pushes prices down further. The market is flooded with options, and pharmacies are incentivized to push the cheapest, most effective choice.
Real People, Real Savings
Andrew Tighe from Phoenix started switching his daughter’s medications to generics after she was diagnosed with a rare condition. Her monthly prescription cost dropped from $500 to under $40. “We saved hundreds a year,” he told ABC15. “It made the difference between keeping her on medication or skipping doses.”
On Reddit, users in r/personalfinance regularly share stories like this:
- “Switched from brand-name Adderall to generic amphetamine salts. Cost went from $150/month to $8. I haven’t missed a dose since.”
- “My dad’s cholesterol med was $120/month. Generic? $3. We’re saving $1,000 a year just on that one pill.”
These aren’t rare cases. They’re common. A 2023 study in JAMA Health Forum found that patients using the Mark Cuban Cost Plus Drug Company (MCCPDC) saved a median of $4.96 per prescription. Uninsured patients saved the most-$6.08 on average. Even people with private insurance saw savings of $3.69 per script.
What About Quality and Effectiveness?
Some people worry generics don’t work as well. They say, “I feel different on the generic.” But here’s what’s really happening: the active ingredient hasn’t changed. What has changed is the pill’s color, size, or inactive ingredients-like dyes or fillers. Sometimes, those differences cause minor side effects like stomach upset or headaches. But they don’t affect how well the drug treats your condition.
For most people, switching to a generic causes zero change in how they feel. For the few who notice a difference-usually with drugs that have a narrow therapeutic index, like levothyroxine or warfarin-it’s not because the generic is weaker. It’s because even tiny shifts in absorption can matter. In those cases, doctors can note “dispense as written” on the prescription to prevent substitution. But for 97% of prescriptions, generic substitution is not just safe-it’s standard.

How to Start Using Generics
You don’t need a PhD to save money on prescriptions. Here’s how to begin:
- Ask your pharmacist: “Is there a generic version of this?” They’re trained to know-and they’ll tell you.
- Check your insurance formulary. Most plans have lower copays for generics. Sometimes, the brand-name drug isn’t even covered.
- Compare cash prices. At Costco, Walmart, or Sam’s Club, generics often cost less than your insurance copay. For example, a 30-day supply of metformin 500mg can be $4 at Costco-no insurance needed.
- Consider alternatives like the Mark Cuban Cost Plus Drug Company. They sell generics at transparent prices: cost + 15% markup. No middlemen. No hidden fees.
- If you’re on Medicare Part D, use the Medicare Plan Finder tool. Many plans have $0 or $5 copays for Tier 1 generics.
Pharmacists are required by law to substitute generics unless your doctor says otherwise. But if you’re unsure, ask. Many people never realize they’re paying more than necessary because they assume the brand-name is better. It’s not.
What About Complex Drugs Like Biologics?
Some drugs, especially those made from living cells-like insulin, rheumatoid arthritis treatments, or cancer drugs-are harder to copy. These are called biologics. They don’t have true generics. Instead, they have biosimilars-drugs that are highly similar, but not identical. Biosimilars are still much cheaper than the original brand. For example, a biosimilar to Humira can cost 40-70% less. The FDA is approving more biosimilars every year, and prices are expected to drop further by 2027 as more patents expire.
For now, if you’re on a biologic, ask your doctor: “Is there a biosimilar available?” You might be surprised at how much you can save.
Why This Matters Beyond Your Wallet
Cost isn’t just about money. It’s about health. When people can’t afford their meds, they skip doses, cut pills in half, or stop taking them entirely. That leads to hospital visits, complications, and even early death. Generics fix that. They make chronic disease management possible for millions who couldn’t otherwise afford it.
They also free up money in the healthcare system. Every dollar saved on a generic is a dollar that can go toward new research, better equipment, or expanded care. The FDA estimates that expanding generic use could save the U.S. healthcare system $100-200 billion annually by 2030.
It’s not just about being cheap. It’s about being smart.
Are generic medications as effective as brand-name drugs?
Yes. The FDA requires generics to deliver the same amount of active ingredient into your bloodstream at the same rate as the brand-name version. This is called bioequivalence. Thousands of studies confirm that generics work just as well. For 97% of prescriptions, there’s no meaningful difference in effectiveness.
Why do generic pills look different?
Generics must have different colors, shapes, or markings because U.S. law prohibits them from looking exactly like the brand-name drug. This prevents confusion. But the active ingredient is identical. The differences are only in inactive ingredients like dyes or fillers-which don’t affect how the drug works.
Can I ask my doctor to prescribe generics only?
Absolutely. You can request that your doctor write "dispense as written" or "generic required" on the prescription. Most doctors will agree, especially for chronic conditions like diabetes, high blood pressure, or high cholesterol. If you’re concerned about cost, mention it-doctors want you to take your meds consistently.
Are generics safe if I’m on multiple medications?
Yes. Generic drugs are held to the same safety and quality standards as brand-name drugs. They’re manufactured in FDA-inspected facilities and tested for purity, potency, and stability. If you’re on multiple medications, your pharmacist can check for interactions-just like they would with brand-name drugs.
What if my insurance won’t cover a generic?
That’s rare, but it can happen if the generic isn’t on your plan’s formulary. Ask your pharmacist to submit a prior authorization request. If that fails, check cash prices at Walmart, Costco, or the Mark Cuban Cost Plus Drug Company. Often, the cash price is lower than your insurance copay.


