When you pick up a prescription, you might not realize that the pill in your hand could be a generic version of a brand-name drug you’ve never heard of. But here’s the thing: if your pharmacist swapped it out, they didn’t just guess. They used something called a Therapeutic Equivalence Code-or TE Code-to make sure it’s safe, effective, and legally allowed to replace the original. These codes are the invisible rulebook behind 9 out of 10 prescriptions filled in the U.S. every year. And if you’ve ever wondered why your expensive brand-name medication suddenly costs $10 instead of $100, TE Codes are why.
What Are TE Codes and Where Do They Come From?
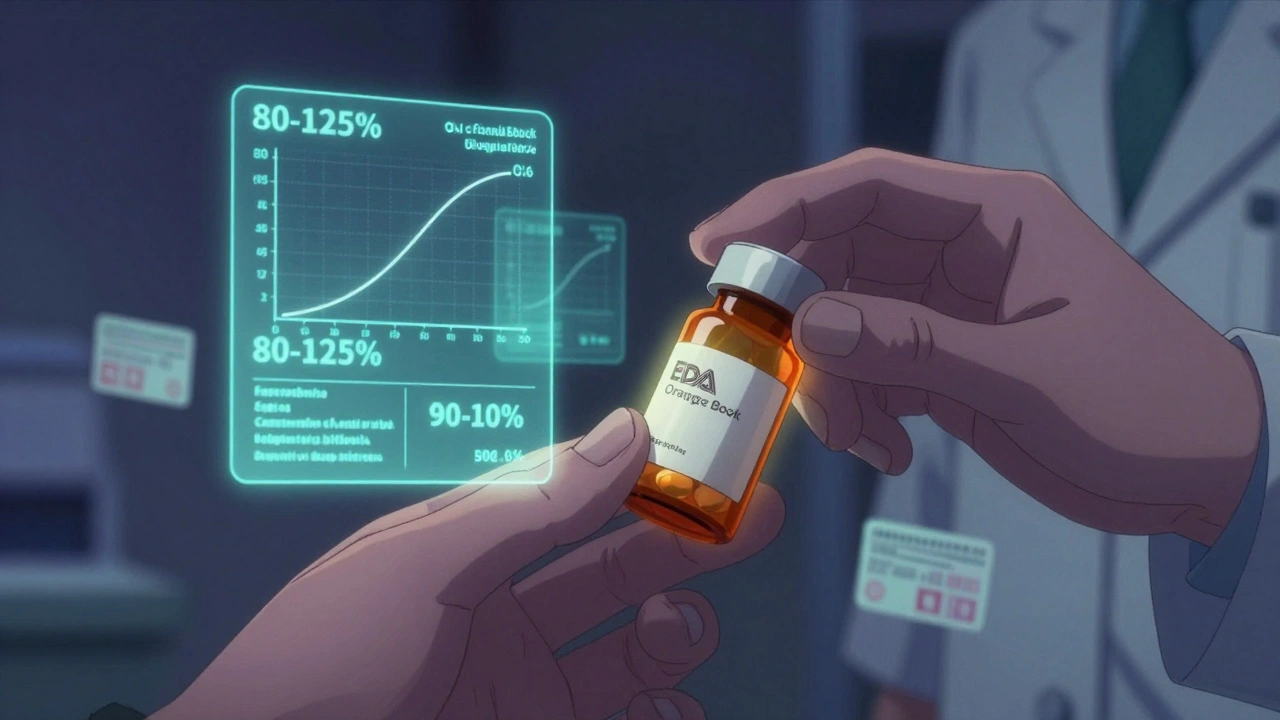
Therapeutic Equivalence Codes are assigned by the U.S. Food and Drug Administration (FDA) and published in a document called the Approved Drug Products With Therapeutic Equivalence Evaluations-better known as the Orange Book. First introduced in 1984 after the Hatch-Waxman Act, TE Codes were created to fix a messy problem: pharmacists didn’t have clear rules about which generics could be swapped for brand-name drugs. Some states allowed substitution, others didn’t. Some generics worked fine. Others didn’t. Patients got confused. Doctors worried. Insurers lost money.
The solution? A science-backed system that tells pharmacists exactly which drugs are interchangeable. It’s not about price. It’s not about marketing. It’s about whether two pills deliver the same amount of active ingredient into your bloodstream at the same speed and produce the same clinical effect. If they do, the FDA gives them an ‘A’ code. If they don’t, it’s a ‘B’.
How TE Codes Work: The A and B System
Every TE Code starts with a letter: A or B. That’s it. But it tells you everything you need to know.
- A means the drug is therapeutically equivalent to the brand-name version. It’s approved for automatic substitution. Your pharmacist can swap it without asking your doctor.
- B means the drug is not considered equivalent. It might have the same active ingredient, but the way it’s absorbed or released in your body is different enough to matter. These aren’t approved for substitution.
After the A or B, there’s usually a second letter-or sometimes two-that gives more detail. For example:
- AA = powder for oral solution (like some antibiotics)
- AN = injectable solution
- AP = powder for injection
- AT = topical cream
These codes help pharmacists match the exact dosage form. A generic tablet labeled ‘AP’ can’t be swapped for a brand-name liquid-different forms, different rules. But two different generic tablets both labeled ‘AA’? Those are interchangeable.
How the FDA Decides What Gets an ‘A’
Getting an ‘A’ isn’t easy. Generic drug makers have to prove three things:
- Pharmaceutical equivalence-the generic has the same active ingredient, strength, dosage form, and route of administration as the brand.
- Bioequivalence-the generic releases the drug into your bloodstream at the same rate and amount as the brand. This is tested with blood samples from healthy volunteers. The FDA requires the generic’s absorption to be within 80-125% of the brand’s. That’s not a guess. It’s a strict, science-backed range.
- Clinical equivalence-the drug works the same way in real patients. The FDA doesn’t run new clinical trials for every generic. Instead, they rely on the bioequivalence data and the fact that the brand’s safety and effectiveness are already proven.
For most common drugs-like atorvastatin (the generic for Lipitor), metformin, or lisinopril-this system works perfectly. Studies published in JAMA Internal Medicine in 2021 showed no difference in cholesterol reduction or blood pressure control between brand-name and TE-rated generics.
Where TE Codes Fall Short
But not all drugs are created equal. Some are more sensitive than others.
Take warfarin, a blood thinner. A tiny change in how it’s absorbed can mean the difference between a clot and a bleed. Even though two generic warfarin tablets might both have an ‘A’ code, some patients report feeling different after switching. A 2022 study in The American Journal of Managed Care found that 12.7% of patients believed their medication changed after a switch-even when lab tests showed no difference. That’s perception, yes, but it’s real to them.
Then there are complex products: inhalers, topical steroids, and injectables. In 2019, the FDA pulled TE ratings for certain generic budesonide inhalers because patients weren’t getting the right dose. The generic had the same chemical, but the spray pattern, particle size, and delivery mechanism were slightly off. That’s enough to make a difference in asthma control.
That’s why the FDA says clearly: TE Codes don’t mean every patient will respond identically. They mean the drugs are interchangeable from a regulatory and population-level standpoint. For high-risk drugs, doctors often write “Do Not Substitute” on the prescription. Pharmacists respect that.
Why TE Codes Matter for You
Let’s say you’re on a brand-name drug that costs $300 a month. The generic version with the same TE code? $15. That’s not a marketing trick. That’s the system working.
Since 1995, TE Codes have helped save the U.S. healthcare system over $2.2 trillion, according to former FDA Director Dr. Janet Woodcock. In 2022 alone, Americans filled 6 billion generic prescriptions-90% of them TE-rated. That’s billions of dollars saved, and it’s not just for people without insurance. Even with Medicare or private plans, lower drug costs mean lower premiums and fewer out-of-pocket surprises.
Pharmacists rely on TE Codes every day. According to the National Community Pharmacists Association, 91% of them feel confident substituting TE-rated generics. Pharmacy software automatically flags which generics are approved. If you’ve ever gotten a generic without asking, that’s TE Codes in action.

What Patients Should Know
You don’t need to memorize codes. But you should know this:
- If your pharmacist switches your medication, they’re following federal and state law-backed by science.
- If you feel different after a switch, tell your doctor. It doesn’t mean the generic is bad. It might mean your body is sensitive to small changes.
- For critical drugs like thyroid meds (levothyroxine), seizure meds, or blood thinners, ask your doctor if substitution is safe for you. Even with an ‘A’ code, some patients do better on one brand or generic than another.
- Check the Orange Book yourself. The FDA’s website lets you search by drug name and see the TE code. You’re not alone if you’re curious.
There’s a myth that generics are “lesser.” They’re not. They’re tested just as hard. The difference is in cost-not quality.
The Future of TE Codes
The FDA is working on updates. In 2024, they plan to extend TE Codes to biosimilars-complex biologic drugs that mimic things like insulin or cancer treatments. Right now, those don’t have codes. That’s changing.
They’re also testing ways to use real-world patient data to improve evaluations. Maybe one day, if 50,000 patients report issues with a certain generic, the FDA will re-evaluate its code. That’s the next step: making TE Codes smarter, not just more numerous.
By 2027, experts predict 93% of all prescriptions will be for TE-rated generics. That’s not just growth-it’s a system that’s working.
Final Thoughts
Therapeutic Equivalence Codes are one of the quietest, most successful public health tools in modern medicine. They let you save money without sacrificing safety. They let pharmacists do their job with confidence. They let insurers keep premiums low. And they let patients get the medicines they need.
It’s not perfect. Complex drugs still challenge the system. Patient experiences vary. But the science behind TE Codes is solid. And for the vast majority of medications-thyroid pills, blood pressure meds, antibiotics, diabetes drugs-it’s the best way to ensure you get the same result, for a fraction of the price.
Next time you pick up a generic, don’t assume it’s a compromise. Assume it’s a victory-for science, for your wallet, and for the healthcare system.
What does an 'A' code mean on a generic drug?
An 'A' code means the generic drug is therapeutically equivalent to the brand-name version. It has the same active ingredient, strength, dosage form, and route of administration, and it delivers the drug into your bloodstream at the same rate and amount. Pharmacists can legally substitute it without asking your doctor.
Can I trust a generic drug with an 'A' code?
Yes. Generic drugs with an 'A' code are held to the same strict standards as brand-name drugs. The FDA requires them to prove bioequivalence through clinical testing and pharmaceutical equivalence. Studies show they work just as well for most people. Over 6 billion TE-rated generics are filled each year in the U.S., with no evidence of widespread safety issues.
Why do some people say they feel different after switching to a generic?
Some patients report feeling different after switching, even when lab results show no change. This can happen with narrow therapeutic index drugs like warfarin, levothyroxine, or seizure medications, where tiny differences in absorption can feel noticeable. It doesn’t mean the generic is ineffective-it might mean your body is sensitive to formulation changes. Always talk to your doctor if you notice a difference.
Are all generic drugs assigned a TE code?
No. Only multi-source drugs-those with more than one manufacturer-are evaluated for TE codes. Single-source generics (where only one company makes the generic) aren’t rated. Also, complex products like inhalers, injectables, and topical creams may not get a code if the FDA can’t confirm equivalence. Always check the Orange Book to see if your drug has a TE code.
How do I find out if my drug has a TE code?
You can search the FDA’s Orange Book online for free. Just enter your drug’s name (brand or generic) and look for the 'Therapeutic Equivalence' column. It will show the code-like 'AA' or 'AP'. Your pharmacist can also check this for you. Many pharmacy systems display the code automatically when filling a prescription.