Many people over 65 take five or more medications every day. Some of those pills might not even be helping anymore-but they’re still costing you money. You’re not alone. In Australia, nearly 40% of older adults are on too many drugs, and in the U.S., that number is even higher. The truth? Not every medication you’ve been handed over the years is still necessary. Stopping the wrong ones-called deprescribing-can cut your monthly bills, lower your risk of falls and confusion, and even keep you out of the hospital. And it all starts with a simple conversation with your doctor.
What Deprescribing Really Means
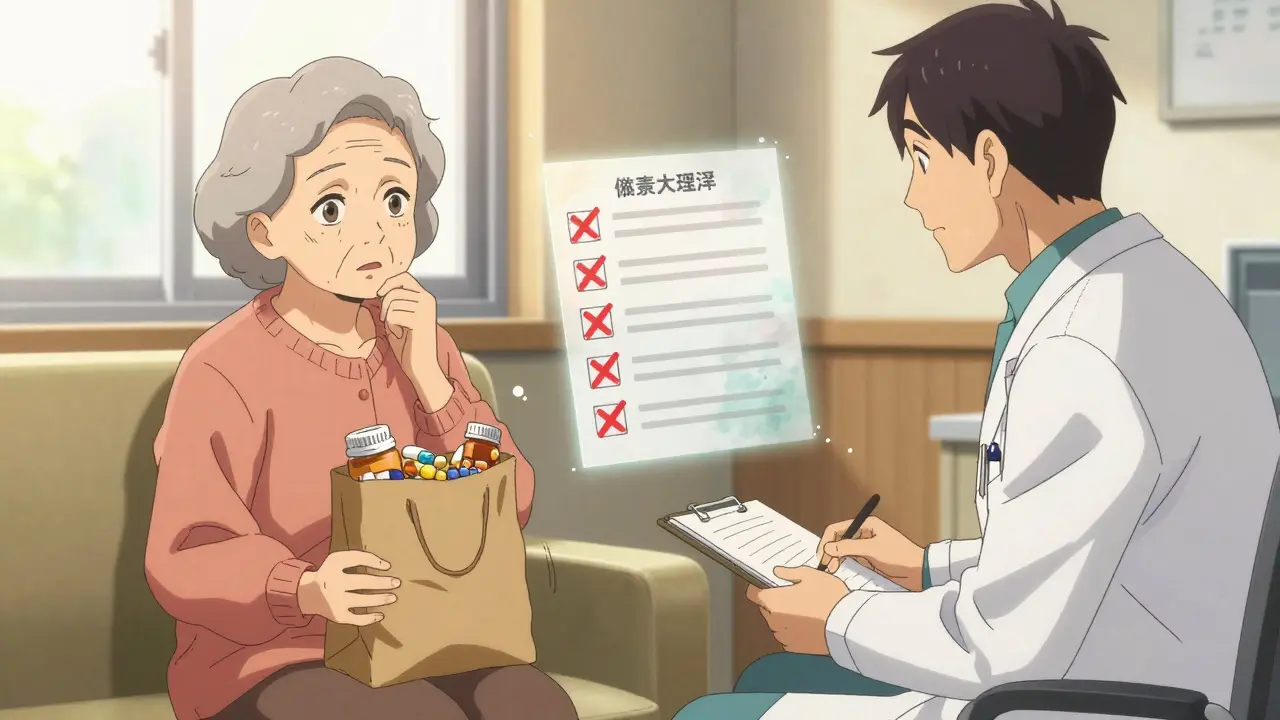
Deprescribing isn’t just quitting pills. It’s a careful, step-by-step process of reviewing your medications to find the ones that no longer do more good than harm. It’s not about stopping everything. It’s about removing the ones that are outdated, redundant, or risky. Think of it like cleaning out your medicine cabinet: you keep what works, toss what doesn’t, and replace what’s expired. The goal isn’t to feel better overnight. It’s to feel safer and lighter-both physically and financially. A 2022 study found that people who stopped one unnecessary $50-a-month medication saved $600 a year. Multiply that by three or four meds, and you’re talking about real cash back in your pocket. Plus, you reduce your chances of side effects like dizziness, memory problems, or stomach bleeding, which can lead to emergency visits costing thousands.Why You’re Taking Too Many Medications
You didn’t get here by accident. Over time, it’s easy to pile on prescriptions. Maybe you saw a specialist who added a drug for a new issue. Then your GP kept it because no one asked to review it. Maybe you started a supplement because a friend swore by it. Or you kept taking a pill because you assumed it was still needed. Polypharmacy-taking five or more medications-is common. But it’s not harmless. For people over 65, nearly one in three hospital admissions is linked to medication problems. Many of these are preventable. A 2021 study showed that 37% of medication-related hospitalizations in older adults could have been avoided with proper review. That’s not just a health risk-it’s a financial one. A single avoidable hospital stay can cost over $15,000. That’s more than most people spend on meds in a year.How to Prepare for Your Deprescribing Conversation
Don’t walk into your doctor’s office with a vague feeling that you’re on too many pills. Come prepared. The most effective way to start this conversation is with a complete list of everything you take. Make a list that includes:- Every prescription (name, dose, why you take it)
- Every over-the-counter drug (pain relievers, antacids, sleep aids)
- All vitamins, herbs, and supplements
- The cost of each (check your pharmacy receipt or app)
Questions to Ask Your Doctor
Once you’ve got your list, ask these five questions for every medication:- Why am I taking this? (What problem is it supposed to fix?)
- What happens if I stop it? (Could my condition get worse-or could I feel better?)
- Can this cause falls, confusion, or dizziness?
- Is there a cheaper or safer alternative?
- Can we try stopping or lowering the dose? How would we monitor it?

What Happens When You Stop a Medication
You can’t just quit cold turkey. Some meds need to be tapered slowly. Stopping blood pressure or antidepressant pills too fast can cause rebound effects-like a spike in blood pressure or worsened anxiety. That’s why deprescribing is a process, not a one-time event. Your doctor might suggest:- Stopping one medication at a time
- Reducing the dose first, then stopping
- Monitoring symptoms for 4 to 12 weeks
- Scheduling a follow-up in 1 to 2 months
Who Else Can Help?
You don’t have to do this alone. Your pharmacist is a secret weapon. Most community pharmacies in Australia and the U.S. offer free Medication Therapy Management (MTM) under Medicare or similar programs. Pharmacists review your entire list, spot duplicates, flag interactions, and suggest cheaper alternatives. One 2022 study found that pharmacists identified an average of $1,200 in annual savings per patient just by reviewing prescriptions. They might suggest switching from a brand-name statin to a generic, or stopping a supplement that’s not backed by science. If you’re seeing multiple doctors, ask for a single point person-usually your GP-to coordinate everything. Fragmented care is one of the biggest reasons people end up on too many meds.Real Savings, Real Stories
A 72-year-old woman in Ohio stopped three medications after a brown bag review: a $120/month sleep aid she didn’t need, a $45/month supplement her cardiologist said was redundant, and a $50/month antacid that was causing more stomach issues than it solved. Her annual savings: $840. She also stopped feeling foggy in the mornings. Another man in Sydney cut his costs by $1,980 a year after his pharmacist pointed out his $90/month vitamin D supplement was unnecessary-his blood test showed normal levels. He also stopped an herbal remedy that interacted with his blood thinner. These aren’t rare cases. They’re common outcomes of structured reviews. Kaiser Permanente’s deprescribing program saved $1.2 million in one year across thousands of patients. That’s not charity-it’s smart medicine.
When Deprescribing Isn’t Safe
Not every drug can-or should-be stopped. Some medications serve multiple purposes. For example, a beta-blocker might be used for high blood pressure and also to prevent migraines. Stopping it could trigger headaches. Or a low-dose aspirin might be prescribed for heart protection, even if you don’t have symptoms. That’s why you need professional guidance. The Beers Criteria-a widely used list of potentially inappropriate medications for older adults-helps doctors identify risky drugs. But it’s not a checklist. It’s a starting point. Your doctor will weigh your health history, age, kidney function, and other factors before making a decision.What to Do If Your Doctor Says No
Sometimes, doctors say no because they’re rushed. A typical GP visit in Australia lasts about 15 minutes. That’s not enough time to review 10 medications. If your doctor says “it’s fine,” ask: “Can we schedule a longer appointment just for meds?” or “Can you refer me to a pharmacist for a free medication review?” If they still refuse, get a second opinion. Bring your list to another GP or a geriatrician. Many hospitals now have medication review clinics. You can also ask your local pharmacy if they offer free MTM services. Don’t give up. You’re not being difficult-you’re being responsible.The Bigger Picture: Why This Matters
Medication costs have risen 60% since 2014. For seniors on fixed incomes, drugs can eat up nearly 20% of their monthly budget. At the same time, preventable medication errors cost the Australian healthcare system hundreds of millions each year. Deprescribing isn’t just personal-it’s systemic. When more people safely stop unnecessary drugs, fewer people end up in hospitals. Fewer hospital visits mean lower insurance premiums and less strain on public health systems. It’s a win for your wallet and your community. The 2023 Inflation Reduction Act in the U.S. capped insulin at $35/month and expanded access to medication reviews. Australia is moving in the same direction. More GPs are being trained. More pharmacists are offering reviews. The tools are here. The knowledge is growing. You just need to start the conversation.Next Steps: Your Action Plan
Here’s what to do right now:- Collect every pill, capsule, and supplement you take. Write down the name, dose, and cost.
- Call your GP and ask for a “medication review appointment.” Say: “I’d like to review all my medications to see if any can be safely stopped to save money and reduce side effects.”
- Book a free Medication Therapy Management session with your pharmacist.
- Ask your pharmacist to check for duplicates, interactions, and cheaper alternatives.
- Start with one medication you suspect is unnecessary-maybe a supplement or an old prescription.
- Track how you feel after stopping it. Keep notes on sleep, energy, digestion, or dizziness.
Is deprescribing the same as stopping all my meds?
No. Deprescribing means carefully reviewing each medication to find the ones that are no longer needed, risky, or redundant. You keep what’s necessary and stop what’s not. It’s not about quitting everything-it’s about simplifying your regimen safely.
Can I stop a medication on my own if I think it’s unnecessary?
No. Stopping some medications suddenly-like blood pressure pills, antidepressants, or steroids-can cause serious side effects, including rebound high blood pressure, anxiety, or seizures. Always work with your doctor or pharmacist to taper off safely.
How much money can I really save by deprescribing?
On average, stopping one unnecessary $50/month medication saves $600 a year. People who stop three or four unnecessary drugs often save $1,000 to $2,000 annually. Plus, avoiding a single medication-related hospital visit can save over $15,000.
Are supplements always unnecessary?
Not always, but many are. For example, vitamin D supplements are often prescribed without checking blood levels. If your levels are normal, the supplement isn’t helping-and it’s costing you. A 2022 study found that 60% of older adults taking vitamin D supplements didn’t need them. Always ask for a blood test before continuing.
What if my doctor doesn’t know about deprescribing?
Many doctors support deprescribing but aren’t trained in how to do it. Bring printed guidelines from the American Academy of Family Physicians or the Deprescribing Network. Ask if they can refer you to a pharmacist or a medication review clinic. You’re not asking them to be an expert-you’re asking them to help you find the right resources.
How often should I review my medications?
At least once a year. But if you’ve had a major health change-like a new diagnosis, hospital stay, or side effect-review them sooner. Also review after seeing a new specialist. Each new prescription should be evaluated in the context of your whole list.