Every year, thousands of people end up in the hospital with severe liver damage-not from alcohol, not from viruses, but from something they thought was safe: acetaminophen. It’s in painkillers, cold medicines, sleep aids, and even some prescription opioids. The problem? Most people don’t realize they’re taking it more than once a day. And that’s how liver injury happens.
Why Acetaminophen Combination Products Are Risky
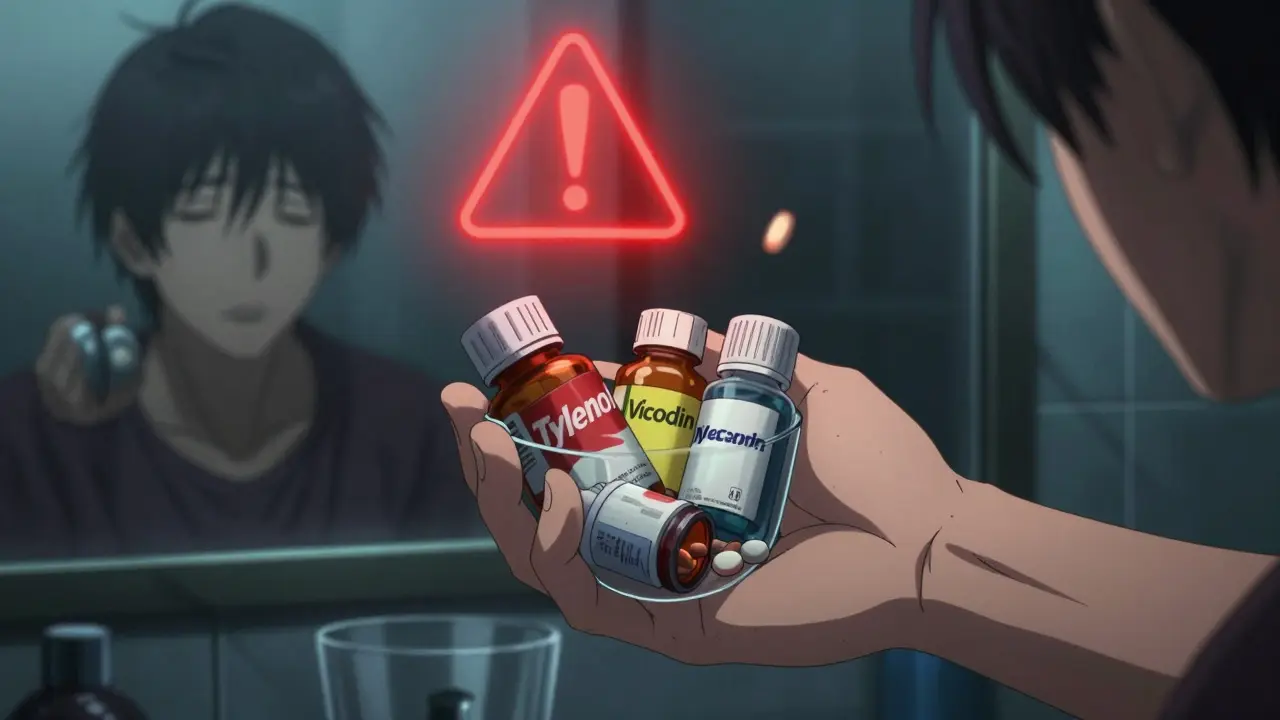
Acetaminophen, also known as paracetamol, is one of the most common pain relievers in the world. You’ll find it in Tylenol, Excedrin, and dozens of prescription brands like Vicodin, Percocet, and Darvocet. These are called combination products because they mix acetaminophen with another drug-usually an opioid like hydrocodone or oxycodone. The danger isn’t the opioid. It’s the acetaminophen. People take one pill for back pain, then another for a headache, then a cold medicine before bed. Each pill has 325 mg or 500 mg of acetaminophen. Add them up, and you’ve easily hit 4,000 mg-the maximum daily limit. But here’s the catch: many don’t know that’s the limit. A 2021 Consumer Reports survey found only 28% of adults knew the correct daily maximum dose. In 2011, the FDA stepped in and forced manufacturers to cap prescription combination products at 325 mg of acetaminophen per tablet. That cut down the risk-but didn’t eliminate it. A 2019 study in Hepatology showed that even after the rule change, combination products still caused nearly 1 in 4 acetaminophen-related liver injuries. And 68% of those cases were unintentional.How Acetaminophen Damages the Liver
Your liver breaks down acetaminophen using two safe pathways: glucuronidation and sulfation. But when you take too much, those pathways get overwhelmed. The extra acetaminophen gets processed by a different enzyme-CYP2E1-which turns it into a toxic byproduct called NAPQI. Normally, your liver has enough glutathione (GSH) to neutralize NAPQI. But when you overdose, glutathione runs out. NAPQI starts attacking liver cells, damaging mitochondria and triggering inflammation. This leads to cell death, liver failure, and sometimes death. The tipping point? When glutathione drops below 30% of normal levels. That can happen after just 10 to 12 hours of taking too much acetaminophen. And once that happens, the damage spreads fast.Who’s at Highest Risk?
Not everyone who takes too much acetaminophen gets liver damage. Some people are more vulnerable.- People who drink alcohol regularly-even a few drinks a day-have lower glutathione levels. Their livers are already stressed.
- People with poor nutrition or eating disorders have less glutathione too.
- Older adults process drugs slower, so acetaminophen sticks around longer.
- People taking multiple medications-especially those with chronic pain, insomnia, or depression-are more likely to accidentally double up.

How to Prevent Overdose: 5 Practical Steps
1. Know What’s in Every Pill You Take
Check every medication label-prescription and over-the-counter-for “acetaminophen,” “APAP,” or “paracetamol.” Don’t assume it’s just in Tylenol. It’s in DayQuil, NyQuil, Excedrin Migraine, Percocet, and even some cough syrups. If you’re unsure, ask your pharmacist. They can scan your prescriptions and tell you if you’re stacking acetaminophen. A 2021 study found pharmacist-led counseling reduced unintentional overdoses by 41%.2. Never Mix Painkillers Without Checking
If you’re prescribed Vicodin for a broken bone, don’t also take Advil PM for sleep. Advil PM contains acetaminophen. So does Tylenol Cold & Flu. So does Excedrin. Write down every medication you take, including OTCs. Then check the acetaminophen content in each. Add it up. If you’re over 3,000 mg, talk to your doctor.3. Use Only One Acetaminophen Product at a Time
If you need pain relief, pick one product with acetaminophen and stick with it. Don’t rotate between different brands thinking you’re “giving your liver a break.” That’s a myth. Every pill adds to the total. If you need something stronger, ask your doctor about alternatives that don’t contain acetaminophen-like tramadol or non-opioid options.4. Use Technology to Track Your Dose
New tools are helping people avoid mistakes. In 2023, the Acetaminophen Hepatotoxicity Prevention Consortium launched a smartphone app that scans barcodes on medication bottles and calculates your total daily acetaminophen intake. Beta testers got it right 89% of the time across 150 different products. Even simpler: set a daily reminder on your phone. “Did I take acetaminophen today?” If you’re not sure, skip it.5. Ask About NAC Before You Need It
N-acetylcysteine (NAC) is the antidote for acetaminophen overdose. It works by restoring glutathione. But it only works well if given within 8 hours of overdose. After 12 hours, its effectiveness drops sharply. If you’re on long-term acetaminophen therapy, ask your doctor if you should keep NAC on hand. In 2023, the FDA approved a new extended-release NAC tablet that lasts 12 hours instead of 4-making it easier to use at home.What to Do If You Think You’ve Taken Too Much
If you’ve taken more than 7,000 mg in 24 hours-or even 4,000 mg and you’re feeling nauseous, sweaty, or have pain in your upper right abdomen-go to the ER immediately. Don’t wait for symptoms. Doctors use the Rumack-Matthew nomogram to decide if you need NAC. It’s based on your blood acetaminophen level and the time since you took it. If you’re within 8 hours, NAC can prevent liver damage almost entirely. If you’re past 12 hours, newer treatments like fomepizole may help. Approved in 2021, it blocks the enzyme that turns acetaminophen into NAPQI. Studies show it reduces severe liver injury by 32% when given with NAC.
What’s Changing in the Future
The FDA is considering lowering the maximum dose in OTC acetaminophen products from 1,000 mg to 650 mg per tablet. That would make it harder to accidentally overdose with just a few pills. Some researchers are exploring natural compounds like emodin (from rhubarb) and sulforaphane (from broccoli sprouts) that activate the body’s own antioxidant systems. These could one day be added to medications as built-in protection. But experts warn: no pill can replace education. Dr. Hartmut Jaeschke, a leading liver researcher, says the real problem isn’t the drug-it’s polypharmacy and low health literacy. People don’t know what’s in their medicine. And that’s the real danger.Final Thoughts: Safety Starts With Awareness
Acetaminophen is safe when used correctly. But in combination products, it’s easy to lose track. The liver doesn’t warn you until it’s too late. The best protection? Know what you’re taking. Check every label. Talk to your pharmacist. Don’t mix meds unless you’re sure. And if you’re unsure-skip it. Your liver doesn’t have a voice. But you do. Use it.Can I take acetaminophen if I drink alcohol?
If you drink alcohol regularly-even just a few drinks a week-you’re at higher risk for liver damage from acetaminophen. Alcohol lowers your liver’s glutathione levels, making it harder to detoxify acetaminophen. Experts recommend limiting acetaminophen to no more than 2,000 mg per day if you drink alcohol. Some doctors advise avoiding it entirely.
Is Tylenol safer than other acetaminophen products?
No. Tylenol is just one brand of acetaminophen. All acetaminophen products, whether generic or brand-name, contain the same active ingredient. The risk comes from the total amount you take in a day, not the brand. You can overdose on Tylenol just as easily as on a store-brand version.
How do I know if I’ve taken too much acetaminophen?
Early signs include nausea, vomiting, loss of appetite, sweating, and fatigue. But many people feel fine for the first 24 hours-even after taking a dangerous dose. By the time pain or jaundice appears, liver damage may already be advanced. If you suspect an overdose, don’t wait for symptoms. Go to the ER.
Can I take acetaminophen with ibuprofen or aspirin?
Yes, you can safely take acetaminophen with ibuprofen or aspirin because they work differently in the body. But be careful: many combination cold and flu products already contain acetaminophen. If you take those along with ibuprofen, you might still be overdosing on acetaminophen without realizing it. Always check the labels.
Are children at risk from acetaminophen combination products?
Children are rarely prescribed opioid-acetaminophen combinations. But they can still overdose on OTC acetaminophen products if dosed incorrectly. Always use the measuring device that comes with the medicine. Never use a kitchen spoon. For kids, the maximum dose is based on weight-not age. Ask your pediatrician for the correct amount.
What if I accidentally took too much but feel fine?
Feeling fine doesn’t mean you’re safe. Liver damage from acetaminophen can take 24 to 72 hours to show symptoms. If you’ve taken more than 7,000 mg in 24 hours-or even 4,000 mg and you’re unsure-call poison control (1-800-222-1222) or go to the ER. Time matters. The sooner you get treatment, the better your chances of avoiding permanent damage.