Drug Reaction Assessment Tool
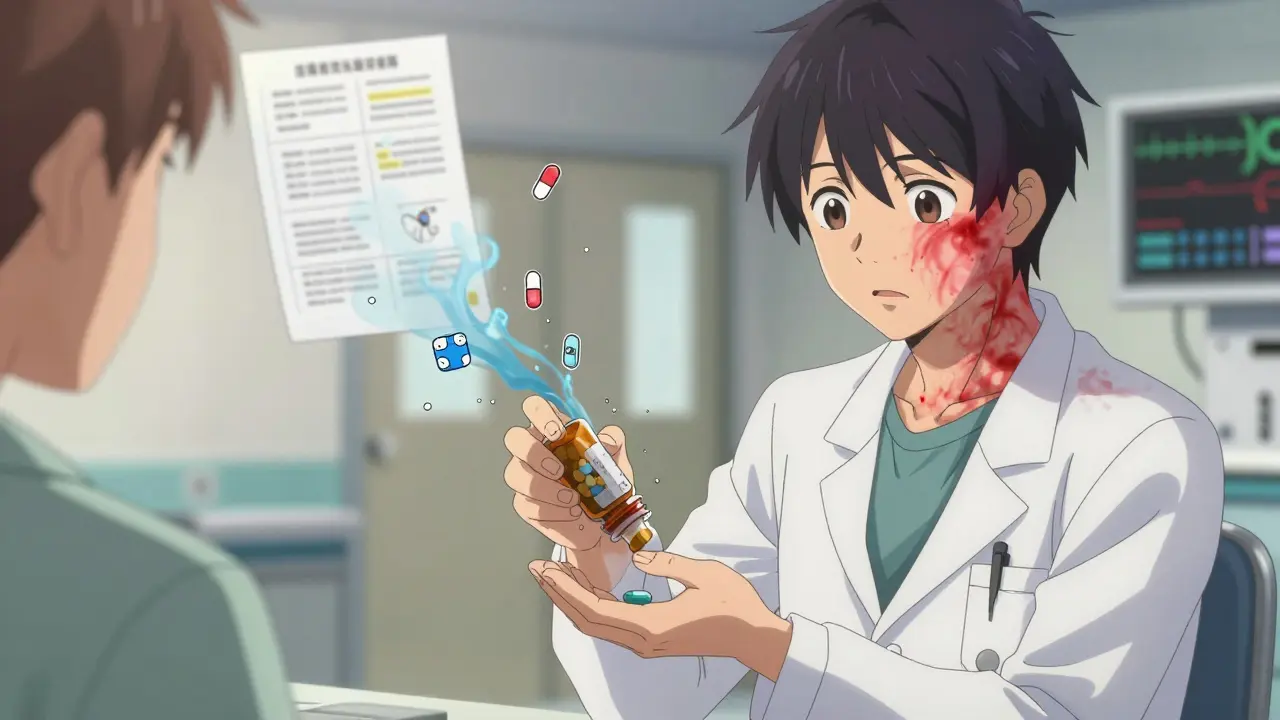
Assess Your Drug Reaction
Enter details about your symptoms and medication use to understand the likelihood that your reaction was caused by the drug.
Result
Important Safety Note
When a patient develops a strange rash, dizziness, or nausea after starting a new medication, doctors don’t just assume it’s the drug’s fault. They need proof. That’s where dechallenge and rechallenge come in-two simple but powerful clinical tools that help separate real drug reactions from coincidence.
What Is Dechallenge?
Dechallenge is the act of stopping a suspected drug to see if the side effect goes away. It sounds basic, but it’s one of the most reliable ways to tell if a medication is actually causing the problem. For example, imagine someone starts taking a new antibiotic and develops a painful, itchy rash two days later. The doctor stops the antibiotic. If the rash fades over the next week, that’s a positive dechallenge. It doesn’t prove the drug caused it 100%, but it strongly suggests it. The timing matters. A good dechallenge shows improvement within a timeframe that matches how long the drug stays in the body. If the drug has a short half-life-like ibuprofen, which clears in 6-8 hours-you’d expect symptoms to improve within a day or two. If it’s a long-acting drug like fluoxetine, it might take two weeks. If symptoms don’t improve after that, the drug is probably not the culprit. But here’s the catch: patients often stop meds on their own. They feel bad, so they quit. That’s not a real dechallenge. For it to count, the stop must be planned, monitored, and documented. Otherwise, you can’t tell if the improvement was due to stopping the drug or just time.What Is Rechallenge?
Rechallenge is when the same drug is given again-on purpose-to see if the side effect comes back. If it does, that’s the gold standard for proving a drug caused the reaction. Take a case from dermatology: a patient develops a fixed drug reaction-a dark, circular rash that always appears in the same spot after taking metronidazole. After stopping the drug, the rash clears. Weeks later, under strict medical supervision, the doctor gives the patient metronidazole again. Within 48 hours, the exact same rash reappears in the same spot. That’s a positive rechallenge. It’s not just correlation-it’s confirmation. Rechallenge is rare. Why? Because it’s risky. If the reaction was severe-like liver failure, Stevens-Johnson syndrome, or anaphylaxis-re-exposing the patient could be deadly. That’s why it’s only done in controlled settings, with emergency equipment ready, and only for mild to moderate reactions. Regulatory agencies like the FDA and EMA allow rechallenge in fewer than 0.3% of serious adverse event reports. Even then, it needs approval from an ethics committee and informed consent from the patient.Why These Tests Matter
Doctors see hundreds of side effect reports every year. Most are just guesses. Dechallenge and rechallenge turn guesses into evidence. The World Health Organization’s causality assessment system uses these tests to classify reactions:- **Probable**: Positive dechallenge, no rechallenge
- **Definite**: Positive dechallenge + positive rechallenge
- **Possible**: No dechallenge or rechallenge, just timing and plausibility
- **Unlikely**: Symptoms didn’t improve after stopping the drug

What Happens When Dechallenge Fails?
Sometimes, symptoms don’t go away after stopping the drug. That’s a negative dechallenge. It usually means one of three things:- The drug wasn’t the cause
- The damage is permanent (like some types of nerve injury or liver scarring)
- Another drug or condition is still causing the problem
Modern Tools Are Helping, But Not Replacing
Technology is making dechallenge easier. Wearable sensors can now track heart rate, skin temperature, and inflammation markers in real time after a drug is stopped. In a 2022-2023 study, sensors detected resolution of side effects in 78% of cases-compared to just 52% when patients just reported how they felt. Scientists are also developing blood tests that predict who’s likely to react to a drug. One test, using lymphocyte toxicity assays, can predict skin reactions with 89% accuracy. That means doctors might soon avoid rechallenge entirely by testing a patient’s cells in a lab instead of risking their health. But experts agree: no algorithm or lab test can replace watching a patient actually get better after stopping a drug. As one WHO expert put it, “No algorithm can substitute for the clinical reality of symptom resolution.”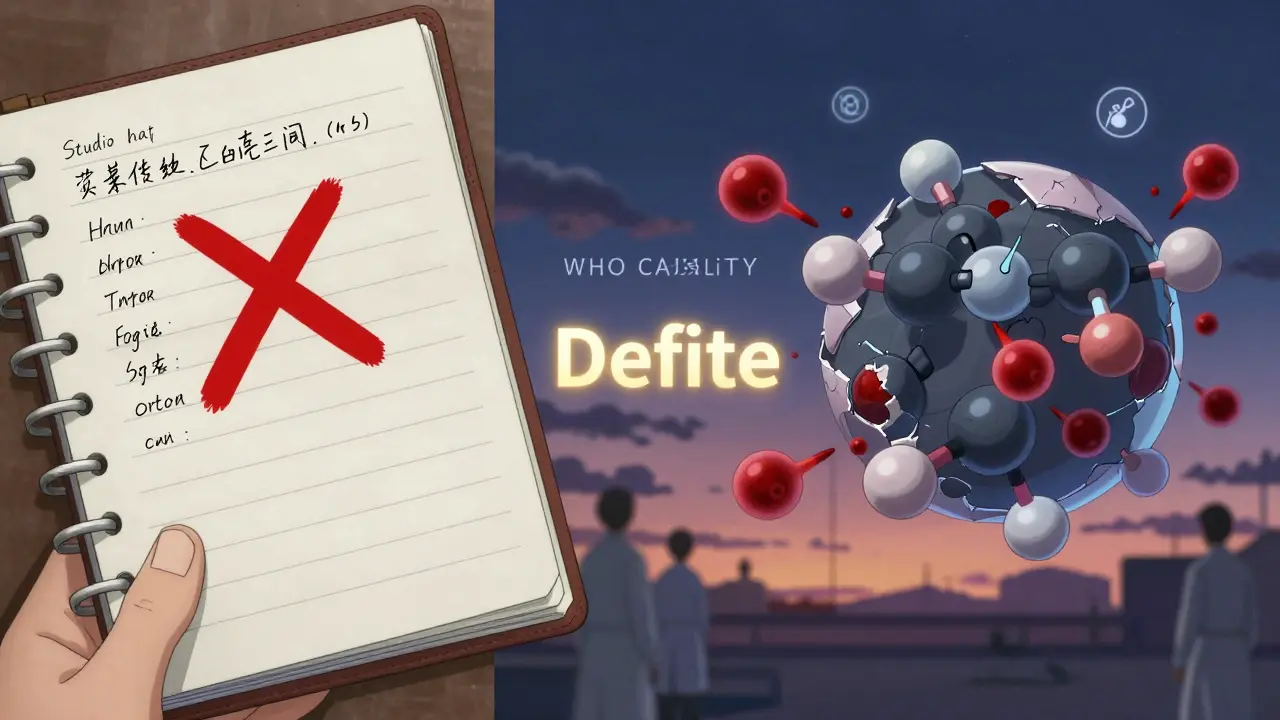
What Patients Should Know
If you’re told to stop a medication because of a side effect, don’t just quit cold turkey-unless it’s an emergency. Talk to your doctor. Ask: “Is this a known reaction? Should I be monitored?” If you’ve had a reaction before, keep a record. Note the drug name, when you took it, what happened, and how long it took to clear. That info could save your life next time. And never, ever ask your doctor to rechallenge you. That’s not something you decide-it’s a medical decision made only under strict safety rules.How the Industry Uses This Data
Pharmaceutical companies are required by law to report all suspected side effects. In 2024, the FDA and EMA updated their reporting systems to demand clear dechallenge outcomes in every submission. If a report doesn’t say whether the drug was stopped or if symptoms improved, it gets flagged. Companies now use software that automatically flags cases with positive dechallenge/rechallenge patterns. This helps them spot dangerous drugs faster. In fact, 82% of major drugmakers now require dechallenge data in post-market safety studies. The global pharmacovigilance market-worth $12.7 billion in 2023-is growing because of this. Better data means safer drugs. And dechallenge and rechallenge are at the heart of it.Bottom Line
Dechallenge and rechallenge aren’t fancy lab tests. They’re simple, old-school clinical observations. But they’re among the most powerful tools we have to figure out what’s really making people sick. They turn suspicion into certainty. They protect patients. They guide drug safety decisions worldwide. And even with all the new tech, they’re still the gold standard. If you’ve ever had a bad reaction to a drug, you’ve already lived through dechallenge. Now you know what it means-and why it matters.Can dechallenge and rechallenge be done at home?
No. Dechallenge should only be done under medical supervision to ensure safety and accurate monitoring. Rechallenge is never done at home-it’s a high-risk procedure that requires emergency equipment and approval from an ethics committee. Never stop or restart a medication without consulting your doctor.
If my symptoms go away after stopping a drug, does that mean it was definitely the cause?
Not necessarily. A positive dechallenge strongly suggests the drug caused the reaction, but other factors could be involved-like an infection, stress, or another medication. Doctors combine dechallenge results with timing, biological plausibility, and other evidence to make a full assessment. It’s one piece of the puzzle, not the whole picture.
Why is rechallenge so rarely performed?
Rechallenge is risky. If the side effect was severe-like a life-threatening rash, liver failure, or anaphylaxis-giving the drug again could kill the patient. Even for mild reactions, doctors avoid it unless the benefit of confirming the cause outweighs the risk. Most of the time, positive dechallenge alone is enough to avoid future use of the drug.
Can a drug cause a side effect without a positive dechallenge?
Yes. Some reactions cause permanent damage-like hearing loss from certain antibiotics or nerve damage from chemotherapy. Even after stopping the drug, symptoms don’t go away. In those cases, dechallenge is negative, but the drug is still the likely cause. Doctors rely on timing, known side effect profiles, and other evidence to confirm the link.
Are there alternatives to rechallenge for proving drug causality?
Yes. Blood tests like lymphocyte toxicity assays can predict if someone is likely to react to a drug without re-exposing them. Genetic tests can also identify people at higher risk for certain reactions. These are growing in use, but they’re not perfect. Clinical dechallenge remains the most direct and trusted method to confirm a drug caused a reaction.