Talk to Doctor About Generics: What You Need to Know Before Switching
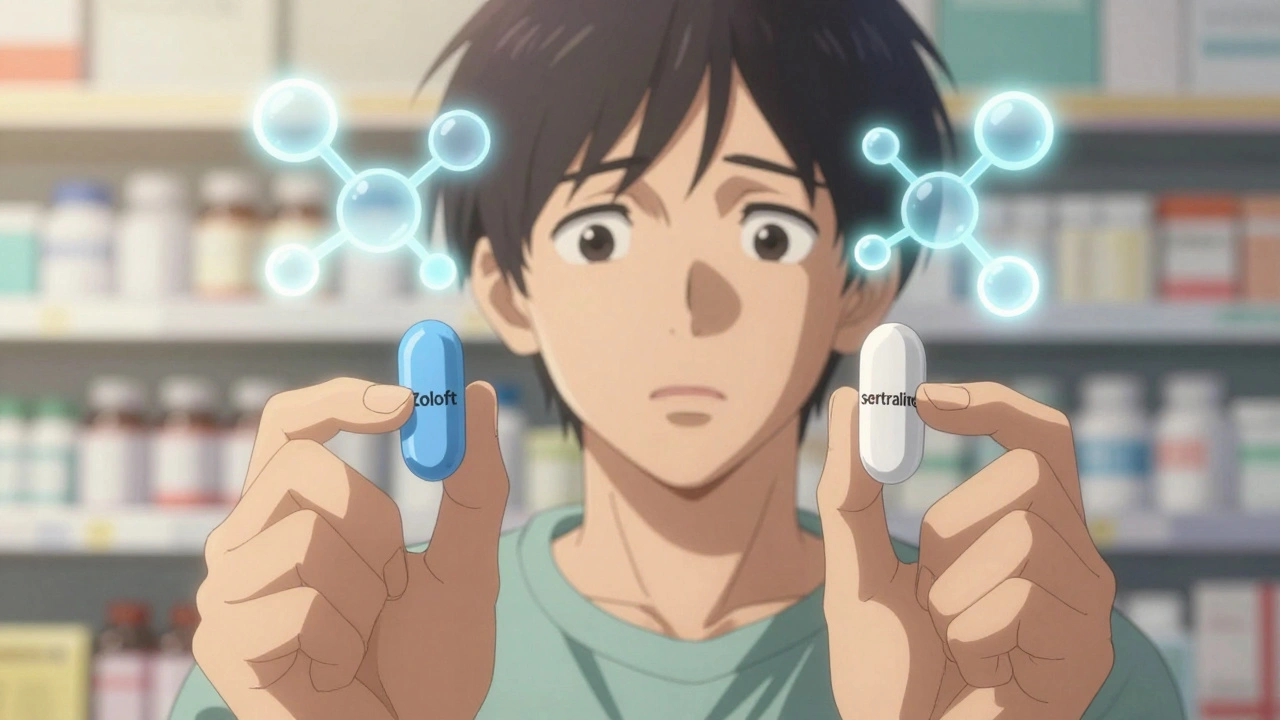
When you hear generic drugs, FDA-approved versions of brand-name medications that contain the same active ingredients, strength, and dosage form. Also known as generic medication, they work the same way as the original—but cost far less. Yet many people still hesitate to switch, unsure if they’re getting the same quality. The truth? Generics aren’t copies. They’re tested, approved, and monitored just like brand-name drugs. The FDA requires them to match the original in how they’re absorbed by your body—this is called bioequivalence testing, a scientific process that proves a generic drug performs identically to its brand-name counterpart in the bloodstream. If your doctor suggests switching, it’s not because they’re cutting corners. It’s because they know you can get the same result at a lower price.
But here’s the catch: switching isn’t always automatic. Some medications need careful handling. For example, if you’re on blood thinners, drugs like warfarin or apixaban that prevent dangerous clots, even tiny differences in how a drug is absorbed can matter. That’s why you never just swap pills without talking to your doctor. Same goes for thyroid meds, seizure drugs, or anything with a narrow therapeutic window. Your doctor doesn’t just prescribe—they help you navigate the fine print. And if you’re unsure whether your prescription is a generic, ask for the label. Pharmacists are required to tell you. You also have the right to written medication instructions, clear, plain-language directions that explain how, when, and why to take each drug. No jargon. No guesswork. Just what you need to stay safe.
Generics aren’t just cheaper—they’re widely used. Over 90% of prescriptions in the U.S. are filled with generics. Billions are saved every year. But savings mean nothing if you’re scared to take them. That fear? It’s often based on myths. One study found patients who switched from brand to generic for high blood pressure had the same results—and were no more likely to end up in the hospital. The same goes for antidepressants, cholesterol meds, and even Parkinson’s treatments. The only time you should avoid generics is when your doctor says so. And even then, it’s usually because of your unique health situation—not because generics are unsafe. So next time you’re handed a new bottle with a different name, don’t assume it’s less effective. Ask: Is this a generic? Is it right for me? What should I watch for? That simple conversation could save you hundreds—and give you peace of mind.
Below, you’ll find real, practical advice on how to ask the right questions, spot red flags, understand how generics are tested, and make sure your switch goes smoothly. Whether you’re on a chronic medication or just curious about saving money, these posts give you the facts—no fluff, no marketing, just what you need to know.
How to Talk to Your Doctor About Generic vs. Brand-Name Medications
- Elliot Grove
- on Dec 4 2025
- 10 Comments