When you pick up your prescription, you might see two names on the label: one you recognize, and another that looks unfamiliar. The brand-name drug you asked for, or a cheaper generic version your pharmacist swapped in without asking. If you’ve ever felt confused or worried about this switch, you’re not alone. Many people assume the cheaper option must be weaker, less reliable, or even unsafe. But here’s the truth: generic medications are not second-rate. They’re exact copies in every way that matters - and they’ve saved patients billions.
Why Generic Drugs Are Just as Effective
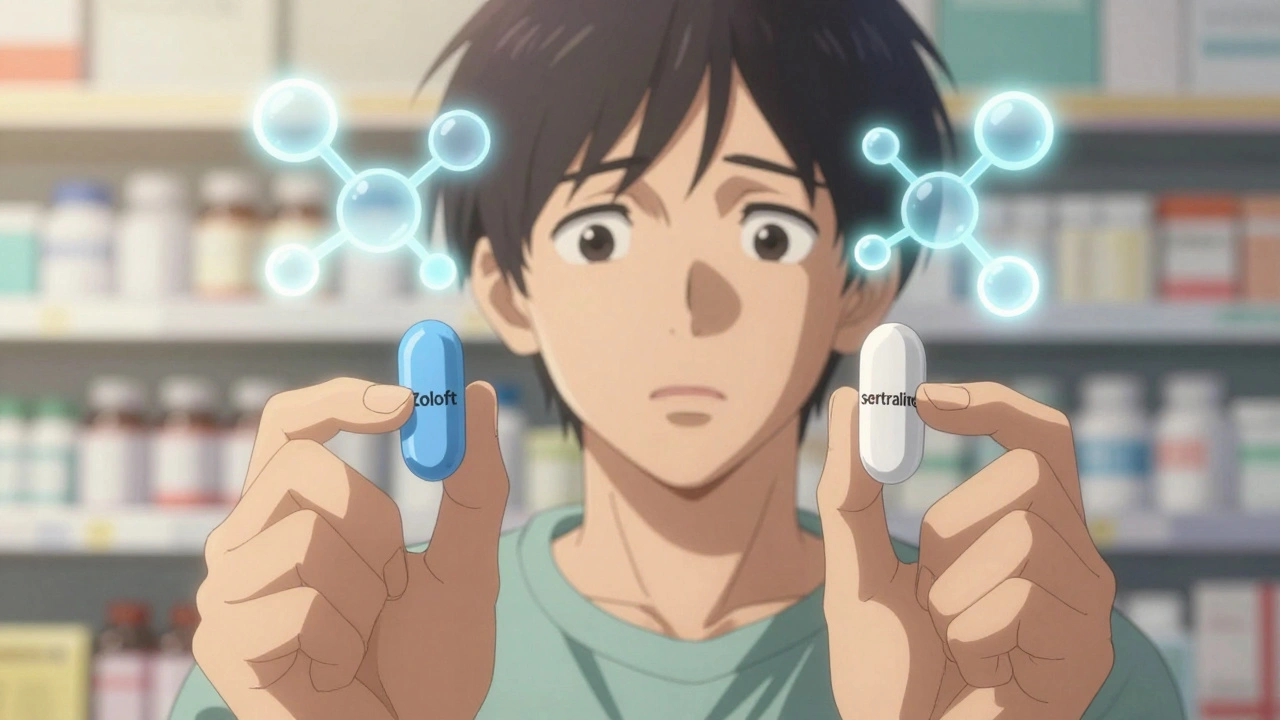
The U.S. Food and Drug Administration (FDA) doesn’t let just any company slap a label on a pill and call it a generic. To get approval, a generic drug must prove it contains the same active ingredient, in the same strength, and works the same way in your body as the brand-name version. That means if you’re taking lisinopril for high blood pressure, the generic version has the exact same molecule as Zestril. The same goes for metformin versus Glucophage, or sertraline versus Zoloft. The FDA requires generics to be bioequivalent - meaning they’re absorbed into your bloodstream at nearly the same rate and amount as the brand. Studies show the average difference in absorption is just 3.5%, well within the FDA’s 20% safety margin. In fact, nine out of ten prescriptions filled in the U.S. are for generics. That’s not because pharmacies are pushing them - it’s because they work just as well.What’s Actually Different Between Generic and Brand-Name Drugs
The real differences? Appearance and price. Generic pills might be a different color, shape, or size. They might have a different taste or coating. That’s because U.S. trademark laws prevent generics from looking identical to brand-name drugs. But none of that affects how the medicine works inside you. The biggest difference is cost. Generics typically cost 80-85% less. A 30-day supply of a brand-name statin might run $150. The generic? $12. Over a year, that’s over $1,500 saved. Between 2007 and 2016, generic drugs saved the U.S. healthcare system more than $1.67 trillion. That’s money that stays in patients’ pockets - and keeps people from skipping doses because they can’t afford their meds.When Your Doctor Might Still Recommend the Brand-Name Version
Most of the time, switching to a generic is safe and smart. But there are exceptions. For drugs with a narrow therapeutic index - where even tiny changes in blood levels can cause serious side effects or treatment failure - some doctors prefer to stick with the brand. Examples include warfarin (for blood clots), levothyroxine (for thyroid), and certain anti-seizure medications like phenytoin. Even here, the FDA says approved generics are safe. But some patients report feeling different after switching - not because the drug changed, but because their body reacted to the change itself. A small number of studies have noted minor fluctuations in blood levels when switching between different generic manufacturers, but these findings are rare and not consistently proven. Most often, what feels like a difference is actually the nocebo effect - where expecting a problem makes you notice it. If you’ve had a bad experience with a generic before, tell your doctor. Don’t assume it’s the drug’s fault. It could be a different filler, dye, or coating that caused a reaction. Your doctor can note “dispense as written” on the prescription if needed.
What to Say to Your Doctor - And What to Ask
Talking to your doctor about medication options doesn’t mean challenging their judgment. It means working together to find the best solution for your health and your budget. Here’s how to start the conversation:- “Is there a generic version of this medication?” - Simple, direct, and common. Most doctors know the answer.
- “Will the generic work just as well for my condition?” - This opens the door for them to explain if there’s any reason to avoid it.
- “I’m on a tight budget. Are there cheaper options?” - Financial stress is a real barrier to taking meds. Doctors can help you find alternatives.
- “I had a reaction to a generic before. Can we check if it’s the drug or the filler?” - This helps them make a more informed choice.
What Happens When the Pharmacy Substitutes Without Asking
In many states, pharmacists are legally required to substitute a generic unless your doctor specifically writes “dispense as written” on the prescription. That means even if you asked for the brand, you might get the generic without a heads-up. That’s not a bad thing - unless you’ve had a bad reaction before. That’s why it’s important to:- Check your pill when you pick it up. If it looks different, ask the pharmacist why.
- Keep a list of all your meds, including what they look like. If the shape or color changes unexpectedly, that’s a red flag to double-check.
- Use your pharmacist as a resource. They’re trained to explain differences and can often clear up confusion on the spot.
Why People Still Doubt Generics - And Why They Shouldn’t
One reason generics get a bad rap? Marketing. Brand-name companies spend millions on ads that make their drugs look superior. But here’s the catch: the FDA doesn’t allow generic manufacturers to advertise their drugs the same way. So you rarely hear about them. Another reason? Change is unsettling. If you’ve been taking a blue pill for years and suddenly get a white one, your brain might think, “This isn’t the same.” But the active ingredient hasn’t changed. The FDA monitors generic manufacturers just as closely as brand-name ones. They inspect factories, test batches, and track side effects. In fact, many brand-name drugs are made in the same factories as generics - just under a different label. Consumer surveys show that 89% of people who switched from brand to generic reported no difference in how the drug worked. And 92% of those who were worried at first said they were satisfied after their pharmacist explained the switch.
What You Can Do Right Now
You don’t need to wait for your next appointment to take control. Here’s what you can do today:- Look up your current prescription on a site like GoodRx. See how much the generic costs versus the brand.
- Check your last few prescriptions. Did the pill look different? If so, note the name and appearance.
- Write down any side effects you’ve noticed since switching - even small ones.
- Bring this info to your next doctor visit. Say: “I noticed my pill changed, and I want to make sure it’s still right for me.”
Final Thought: Cost Isn’t the Only Factor - But It’s a Big One
Medication adherence is one of the biggest problems in healthcare. People skip doses because they’re too expensive. They stop taking pills because they can’t afford refills. Generics fix that. They don’t just save money - they save lives. If your doctor says a brand-name drug is necessary, ask why. If they say a generic is fine, ask if you can try it. Most of the time, you’ll get the same result - for a fraction of the cost. And that’s not just smart. It’s the best kind of healthcare.Are generic medications less effective than brand-name drugs?
No. Generic medications must meet the same strict standards as brand-name drugs. They contain the same active ingredient, work the same way in your body, and are held to the same safety and quality rules by the FDA. Studies show they are just as effective for nearly all conditions.
Why do generic pills look different from brand-name ones?
U.S. trademark laws require generic drugs to look different from brand-name versions. That means different colors, shapes, or markings - but not different ingredients. The active drug inside is identical. These changes are purely cosmetic and don’t affect how the medicine works.
Can switching to a generic cause side effects?
Side effects from switching are rare. Most reported issues are due to the nocebo effect - where expecting a problem makes you notice it. In very rare cases, differences in inactive ingredients (like fillers or dyes) might cause a reaction in sensitive individuals. If you notice a change after switching, talk to your pharmacist or doctor.
Are there any drugs where generics aren’t recommended?
For most drugs, generics are perfectly safe. But for medications with a narrow therapeutic index - like warfarin, levothyroxine, or certain seizure drugs - some doctors may prefer to stick with the brand, especially if you’ve been stable on it. Even then, FDA-approved generics are considered safe. If you’re unsure, ask your doctor if your medication falls into this category.
Can I ask my pharmacist to give me the brand-name drug instead?
Yes - but you may have to pay more. Pharmacists are required by law to substitute generics unless your doctor writes “dispense as written.” If you want the brand, you can request it, but you’ll likely pay the full brand price unless your insurance covers it. Always check with your pharmacist about cost differences before leaving the pharmacy.
How do I know if my generic is from a reliable manufacturer?
All FDA-approved generics, regardless of manufacturer, must meet the same quality standards. The FDA inspects every factory - whether it’s in the U.S., India, or elsewhere - before approving a generic. You can trust any FDA-approved generic. If you’re concerned, ask your pharmacist which company makes your version. They can tell you and reassure you it’s approved.