OSA (Obstructive Sleep Apnea): What You Need to Know
When dealing with OSA, a condition where the airway repeatedly collapses during sleep, causing brief pauses in breathing. Also known as Obstructive Sleep Apnea, it can trigger daytime fatigue, loud snoring, and serious health issues if left untreated.
One of the key players in managing OSA is CPAP therapy, a device that delivers constant positive airway pressure to keep the airway open throughout the night. Alongside CPAP, sleep study, a monitored overnight test that records breathing patterns, oxygen levels, and brain activity provides the data needed to confirm the diagnosis and gauge severity.
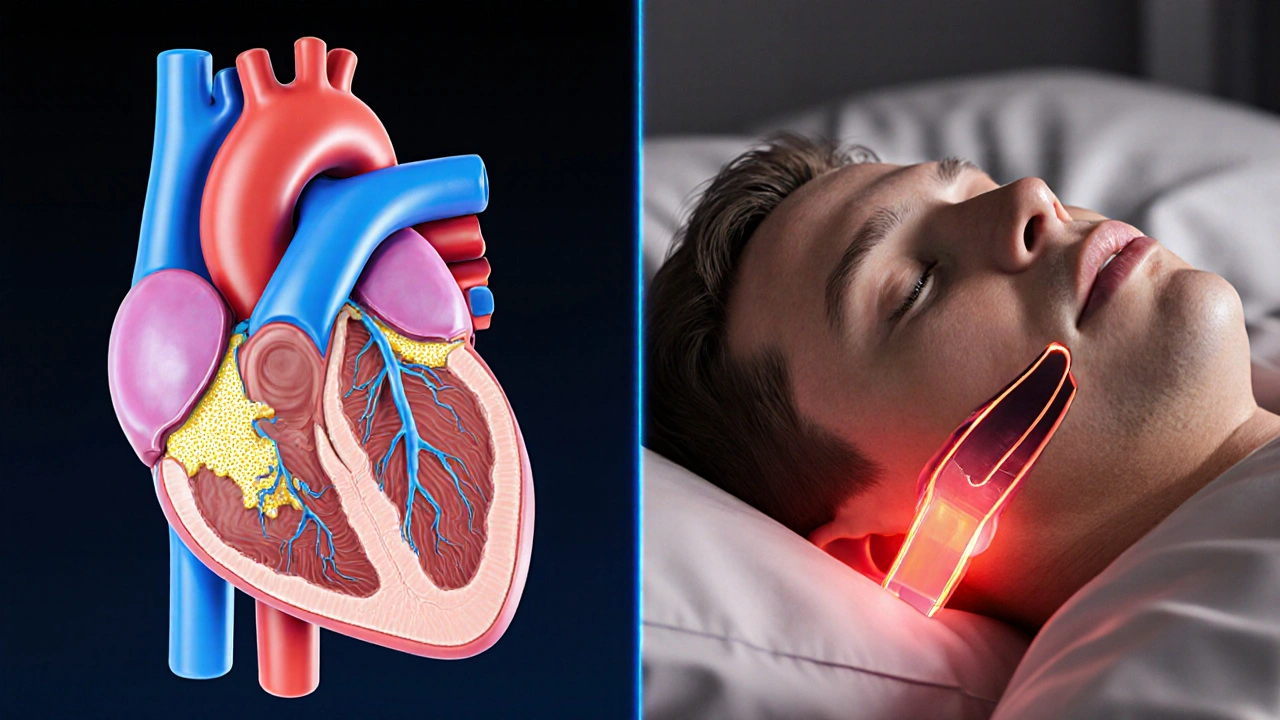
OSA doesn’t exist in a vacuum. Cardiovascular disease, including hypertension and heart failure, often co‑occurs with OSA and can worsen outcomes for both conditions. The relationship is bidirectional: untreated OSA raises blood pressure spikes, while existing heart disease can make airway collapse more likely. Recognizing this link helps clinicians choose the right treatment plan and monitor patients for heart‑related complications.
How OSA Affects Daily Life and What You Can Do About It
People with OSA frequently report morning headaches, irritability, and a hard time staying awake at work. These symptoms stem from repeated drops in blood oxygen during sleep, which trigger the brain’s “wake‑up” response. By using CPAP consistently, most users see a drop in apnea events, better sleep quality, and a noticeable lift in daytime alertness.
Weight management, positional therapy (avoiding sleeping on the back), and treating nasal congestion are practical steps that can reduce the severity of OSA. For those who can’t tolerate CPAP, alternatives like oral appliances or upper airway surgery may be explored, but each option requires a thorough evaluation from a sleep specialist.
Understanding the diagnosis process is essential. A sleep study (either in‑lab or home‑based) records the Apnea‑Hypopnea Index (AHI), which counts breathing interruptions per hour. An AHI of 5–15 indicates mild OSA, 15–30 moderate, and over 30 severe. These numbers guide treatment intensity, insurance coverage, and follow‑up frequency.
Because OSA can accelerate the progression of diabetes, stroke, and chronic kidney disease, regular follow‑ups with both a sleep physician and your primary care doctor are crucial. Monitoring blood pressure, blood sugar, and kidney function helps catch complications early.
Below you’ll find a curated set of articles that dive deeper into each of these topics—from the science behind CPAP machines to lifestyle tweaks that lower apnea risk. Whether you’re just suspecting OSA or already navigating treatment, the collection offers actionable insights you can start using today.
Coronary Artery Disease and Sleep Apnea: How They Influence Each Other
- Elliot Grove
- on Oct 13 2025
- 10 Comments