CAD-Sleep Apnea Risk Assessment Tool
Risk Factors Assessment
This tool estimates your combined risk of coronary artery disease and sleep apnea based on shared risk factors. Answer the questions below for a personalized assessment.
Your Risk Assessment
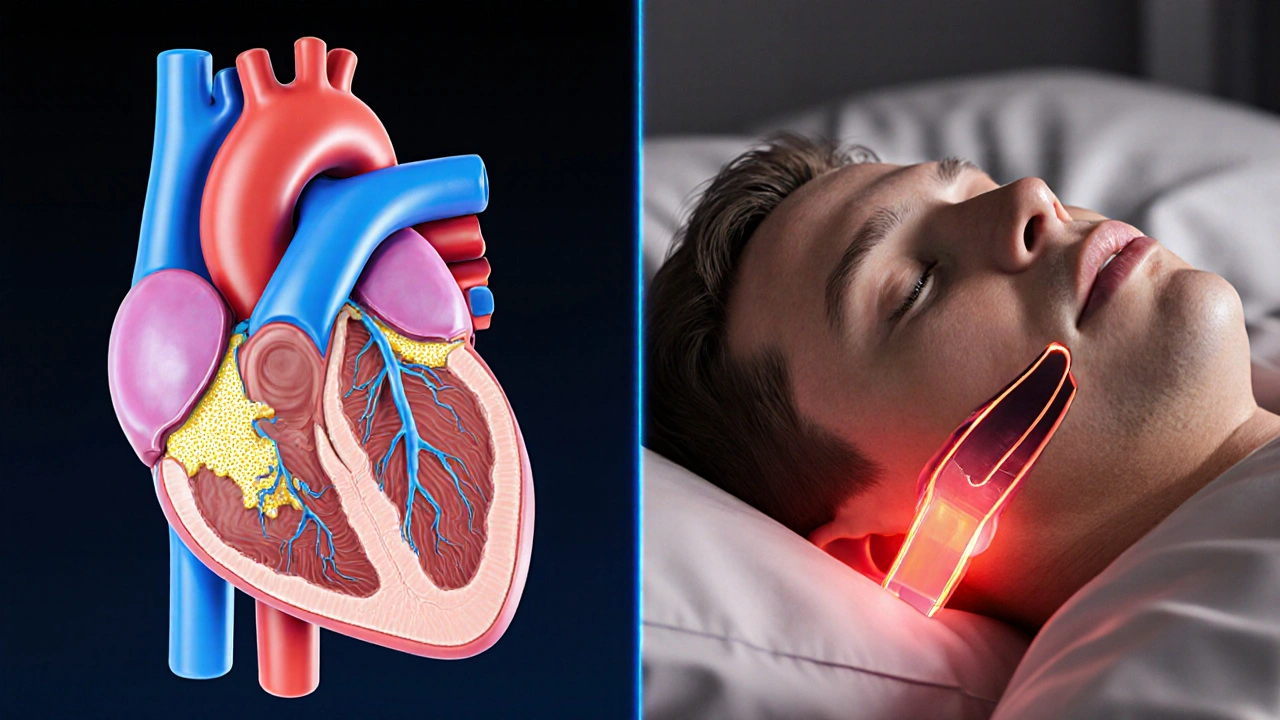
When you hear coronary artery disease is a condition where plaque builds up in the walls of the arteries that supply the heart, making it harder for blood to flow. It can lead to chest pain, heart attacks, and even sudden death. At the same time, sleep apnea is a disorder that repeatedly stops breathing during sleep, often for 10 to 30 seconds at a time. The most common form, obstructive sleep apnea (OSA), occurs when the throat muscles collapse and block the airway. These two problems might seem unrelated, but research over the last decade shows a clear, two‑way connection that can worsen health outcomes if left unchecked.
What Exactly Is Coronary Artery Disease?
Coronary artery disease (CAD) is a type of atherosclerosis that specifically targets the coronary arteries. The disease progresses as low‑density lipoprotein (LDL) cholesterol infiltrates the arterial wall, triggering an inflammatory response. Over time, the plaque hardens, a process called calcification, narrowing the vessel lumen. When the heart muscle doesn’t receive enough oxygen, you may feel angina, or you could suffer a myocardial infarction (heart attack).
Defining Sleep Apnea and Its Main Types
Obstructive sleep apnea (OSA) accounts for roughly 84% of all sleep apnea cases. It happens when soft tissue in the back of the throat collapses during sleep, briefly cutting off airflow. Central sleep apnea (CSA) is less common; it stems from a failure of the brain to send proper breathing signals. Both result in intermittent hypoxia-periods when blood oxygen levels drop-and fragmented sleep.
Why the Heart and Breathing System Talk to Each Other
The link between CAD and sleep apnea is rooted in three physiological pathways:
- Sympathetic activation: Each apnea episode spikes adrenaline, raising heart rate and blood pressure. Repeated surges stress the arterial wall and accelerate plaque growth.
- Endothelial dysfunction refers to the impaired ability of blood vessels to dilate properly. Low oxygen triggers oxidative stress, damaging the endothelium and making it easier for LDL to stick.
- Systemic inflammation is marked by higher C‑reactive protein (CRP) and interleukin‑6 levels. Inflammation fuels the atherosclerotic process and can destabilize existing plaques.
These mechanisms mean that untreated sleep apnea can speed up the progression of CAD, while existing heart disease often makes breathing problems worse by reducing cardiac output during sleep.

Shared Risk Factors: The Overlap Hotspot
Several lifestyle and medical factors raise the odds of both conditions. Recognizing them helps you target prevention.
| Risk Factor | Impact on CAD | Impact on Sleep Apnea |
|---|---|---|
| Obesity | Increases LDL and inflammation | Enlarges neck tissues, narrowing airway |
| Hypertension | Damages arterial wall | Worsens nocturnal blood pressure spikes |
| Diabetes | Accelerates atherosclerosis | Alters neuromuscular control of airway |
| Smoking | Promotes plaque formation | Inflames upper airway |
| Age > 45 (men) / > 55 (women) | Higher plaque burden | Reduced muscle tone in throat |
How Sleep Apnea Changes Heart Health Outcomes
Large cohort studies published between 2018 and 2024 reveal striking numbers:
- Patients with moderate‑to‑severe OSA have a 1.6‑fold higher risk of myocardial infarction compared to those without sleep apnea.
- Untreated OSA raises the likelihood of coronary re‑vascularization procedures by 45% within five years.
- Even after a heart attack, OSA patients experience a 30% higher rate of repeat events.
These stats aren’t just academic-they translate into more hospital stays, higher medication costs, and reduced quality of life.
Detecting Sleep Apnea in Someone With CAD
Because many heart patients don’t realize they snore or pause breathing, proactive screening is essential. Here’s a practical checklist doctors use:
- Ask about loud snoring, witnessed apneas, and daytime fatigue.
- Measure neck circumference - >17inches in men or >16inches in women raises suspicion.
- Utilize the Epworth Sleepiness Scale a questionnaire that scores daytime sleepiness. Scores ≥10 suggest further testing.
- Order a home sleep apnea test (HSAT) or in‑lab polysomnography if risk is high.
- Screen for comorbidities - hypertension, atrial fibrillation, and chronic kidney disease often coexist.
When a CAD patient is found to have OSA, the treatment plan should address both conditions simultaneously.
Treatment Options That Hit Two Birds With One Stone
Effective therapy can lower blood pressure, improve oxygenation, and even stabilize plaque.
- Continuous Positive Airway Pressure (CPAP) delivers steady air pressure to keep the airway open. Randomized trials show CPAP reduces nighttime systolic pressure by an average of 5mmHg and cuts the risk of repeat heart attacks by 20% when used >4hours/night.
- Weight loss programs target the root cause of both OSA and atherosclerosis. A 10% body‑weight reduction can lower apnea‑hypopnea index (AHI) by 30% and improve lipid profiles.
- Medications such as ACE inhibitors help control hypertension and may reduce airway inflammation. Some cardiologists prescribe them alongside CPAP for synergistic blood‑pressure control.
- Dental oral appliances reposition the lower jaw, opening the airway in mild‑to‑moderate OSA; they’re a good alternative for patients intolerant of CPAP.
Regular follow‑up visits-including repeat sleep studies-ensure the chosen therapy remains effective.

Lifestyle Tweaks That Benefit Both Heart and Sleep
Simple daily habits can make a measurable difference:
- Exercise regularly - 150 minutes of moderate aerobic activity per week improves endothelial function and reduces AHI scores.
- Adopt a Mediterranean‑style diet rich in olive oil, nuts, fish, and vegetables. This pattern lowers LDL by 10‑15mg/dL and cuts apnea severity.
- Avoid alcohol and sedatives before bedtime. They relax throat muscles and increase airway collapse.
- Sleep on your side. Side positioning reduces the frequency of apneas by up to 40% compared with supine sleep.
- Maintain a regular sleep schedule. Consistency stabilizes the body’s circadian rhythm, which in turn supports heart rate variability.
When to Call Your Healthcare Provider
If you notice any of these signs, it’s time to seek professional help:
- Chest pain that wakes you up at night.
- Persistent daytime fatigue despite a full night’s sleep.
- Episodes of gasping or choking during sleep observed by a partner. \n
- New onset or worsening hypertension.
- Irregular heartbeats or palpitations.
Early detection and combined treatment can turn a potentially dangerous combo into a manageable health plan.
Bottom Line: Treating One Helps the Other
Because the heart and breathing system are intertwined, ignoring sleep apnea when you have coronary artery disease is like leaving a leak in a roof while the house is already on fire. By screening, diagnosing, and applying therapies that address both problems, patients can lower their cardiovascular risk, improve sleep quality, and enjoy a better overall quality of life.
Frequently Asked Questions
Can sleep apnea cause a heart attack?
Yes. The repeated drops in oxygen and surges in blood pressure during apnea episodes can trigger plaque rupture and clot formation, which are the primary mechanisms behind a myocardial infarction.
Is CPAP the only treatment for sleep apnea in heart patients?
CPAP is the gold standard, but weight‑loss programs, oral appliances, positional therapy, and certain blood‑pressure meds also help. The best approach depends on apnea severity, patient preference, and overall health.
How often should a heart patient be screened for sleep apnea?
Guidelines recommend an initial screen at the time of CAD diagnosis, followed by repeat testing if symptoms change, weight fluctuates by more than 5%, or blood‑pressure control worsens.
Will treating sleep apnea reverse existing heart damage?
It won’t undo scar tissue, but it can halt further progression, improve heart‑failure symptoms, and reduce the chance of new events.
Are there any risks to using CPAP for people with coronary artery disease?
CPAP is generally safe. Rarely, patients may experience nasal dryness, skin irritation, or air‑leak discomfort. These issues are usually managed by adjusting mask fit or humidity settings.