Understanding Nutrient Absorption: How Your Body Takes In Vitamins, Minerals, and Medications
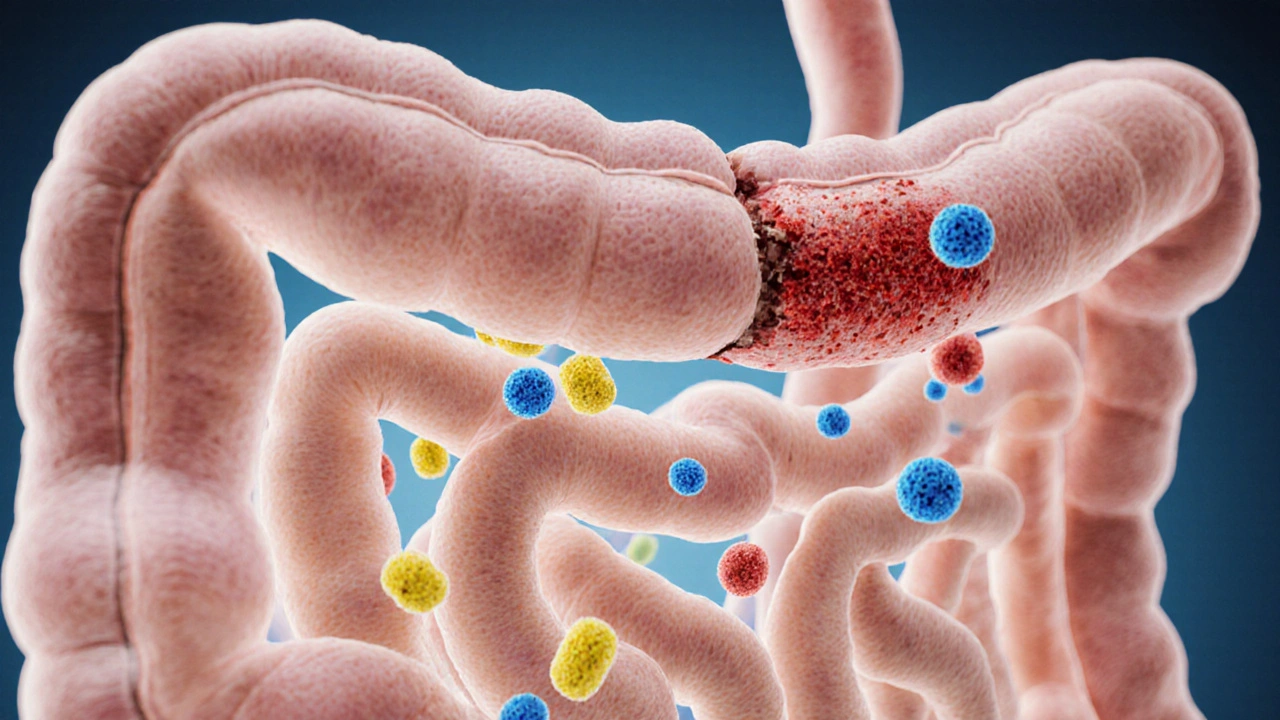
When working with nutrient absorption, the physiological process that moves vitamins, minerals, and other compounds from the digestive tract into the bloodstream. Also known as nutrient uptake, it decides how effectively you power daily activities and how well medicines work. The system nutrient absorption encompasses digestive enzymes, proteins that break down carbohydrates, fats, and proteins into absorbable units, and relies on a balanced gut microbiome, the community of bacteria and fungi that helps process food and modulate immunity. Both of these entities influence how much of a nutrient crosses the intestinal wall. At the same time, drug interactions, situations where medicines alter the absorption of nutrients or vice‑versa can either boost or block that flow. Understanding these links sets the stage for smarter health choices.
Key Factors That Affect Nutrient Absorption
First, enzyme production matters. If your pancreas or small‑intestine doesn’t release enough amylase, lipase, or protease, carbs, fats, and proteins stay in larger pieces that the gut can’t absorb. Conditions like chronic pancreatitis or certain heart drugs, such as Metoprolol, lower gastric acidity and can blunt enzyme activity, meaning fewer nutrients slip through. Second, the gut lining itself can be compromised by common NSAIDs like Celecoxib or the pain reliever Ponstel (mefenamic acid). Those drugs irritate the mucosa, creating tiny gaps that let nutrients leak out or, conversely, let harmful substances in. Third, antibiotics and antiviral meds—think Efavirenz or Ciprofloxacin—shuffle the microbiome balance. When good bacteria dip, the microbiome’s role in breaking down fiber and synthesizing B‑vitamins shrinks, directly lowering absorption rates. Lastly, vitamin and mineral supplements rely on the same pathways. A low‑dose iron pill might compete with calcium from a dairy‑rich meal, while a high‑dose vitamin D supplement needs adequate fat intake to dissolve and be taken up. Each of these examples shows how drug interactions can interfere with the core process, turning a well‑intentioned regimen into a missed opportunity for nourishment.
So, what can you do to keep the system running smooth? Start by pairing meals with the right enzymes—chew thoroughly, consider a probiotic if you’ve taken a course of antibiotics, and check with your pharmacist whether any prescription (like a beta‑blocker or an antiretroviral) might affect your mineral balance. Adjust timing: take iron supplements away from calcium‑rich foods, and schedule NSAIDs with food to protect the gut lining. Monitoring symptoms such as frequent bloating, unexpected fatigue, or changes in stool can hint at absorption problems before they become serious. The articles below dive deeper into specific medications, compare drug classes, and give action‑oriented advice to help you protect and optimize your nutrient uptake. Explore the collection to see how heart medicines, pain relievers, antibiotics, and everyday supplements each play a part in the bigger picture of nutrient absorption.
How Poor Food Absorption Links to Common Gastrointestinal Disorders
- Elliot Grove
- on Oct 14 2025
- 19 Comments