Food Malabsorption: What It Is and How to Manage It
When dealing with food malabsorption, the body’s ability to break down and absorb nutrients from what you eat is compromised. Also known as nutrient malabsorption, it can cause chronic diarrhea, bloating, weight loss, and fatigue. Understanding the underlying reasons helps you pick the right tests and treatments.
Key Factors to Consider
One of the most common triggers is celiac disease, an autoimmune reaction to gluten that damages the small‑intestine lining. Celiac disease requires a strict gluten‑free diet to prevent further damage, and it often presents with iron‑deficiency anemia, bone pain, and skin rash. If you suspect celiac disease, a blood test for tissue transglutaminase antibodies followed by an endoscopic biopsy confirms the diagnosis.
Another frequent cause is lactose intolerance, the inability to digest lactose due to low lactase enzyme activity. Lactose intolerance leads to symptoms like gas, cramping, and watery stools after dairy consumption. A simple hydrogen breath test can pinpoint the issue, and managing it usually means limiting or eliminating lactose‑containing foods.
When nutrients aren’t absorbed properly, nutrient deficiencies, shortages of vitamins and minerals essential for health often follow. Common deficiencies include iron, calcium, vitamin D, and B12, each bringing its own set of problems—iron deficiency causes anemia, calcium loss weakens bones, and B12 shortfall leads to nerve issues. Lab work that checks serum levels guides supplementation and dietary tweaks.
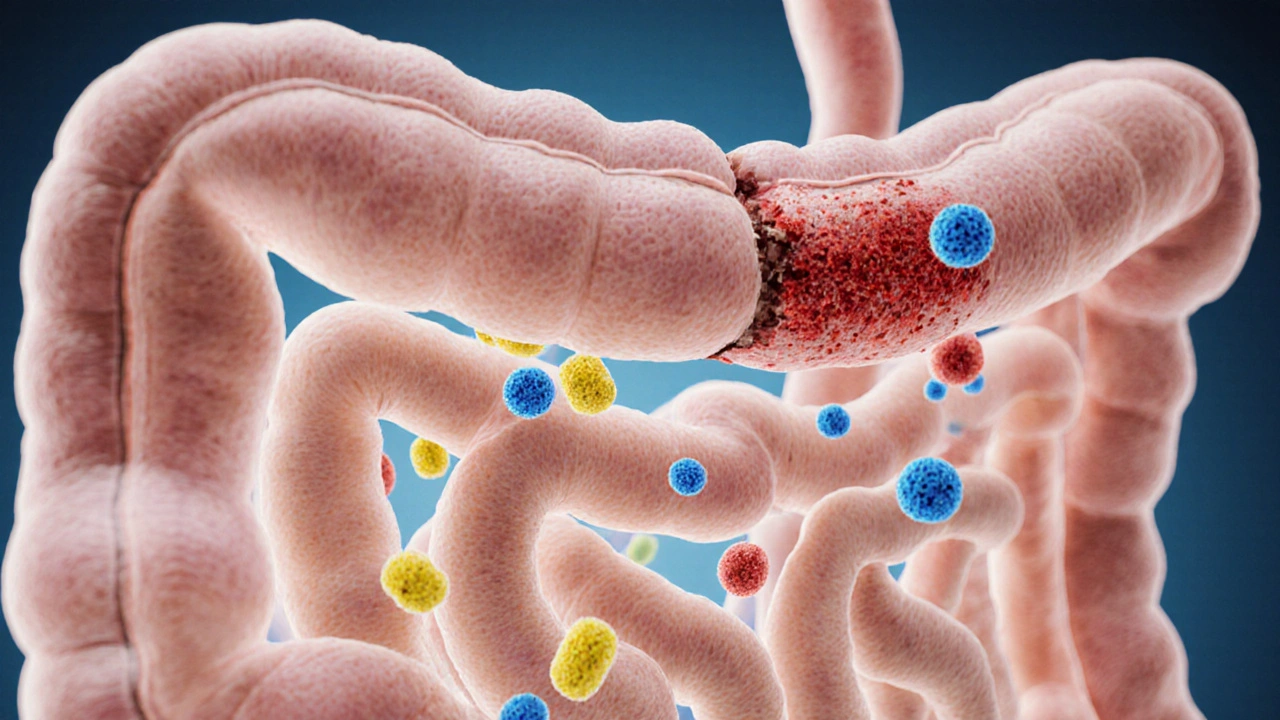
Beyond eliminating problem foods, many people turn to probiotic therapy, the use of live beneficial bacteria to restore gut balance. Probiotics can improve symptoms by enhancing intestinal barrier function and outcompeting harmful microbes. Strains such as Lactobacillus rhamnosus and Bifidobacterium lactis have shown promise in reducing bloating and normalizing stool patterns.
Accurate diagnosis relies on diagnostic testing. Blood panels check for antibodies, iron, vitamin D, and B12 levels. Stool studies evaluate fat content and detect parasites. Imaging and endoscopy may be needed for structural issues. Each test provides a piece of the puzzle, allowing clinicians to tailor a plan that tackles the root cause rather than just the symptoms.
Dietary adjustments remain the cornerstone of treatment. A gluten‑free diet stops celiac‑related damage, while a low‑FODMAP approach can ease IBS‑type malabsorption. For lactose intolerance, lactase enzyme supplements or lactose‑free dairy options keep calcium intake high. Pairing these changes with targeted supplementation and, when appropriate, probiotic use creates a comprehensive strategy that supports healing and prevents relapse.
With the basics covered, you’re ready to explore specific medications, supplements, and lifestyle tips that can make a real difference. Below you’ll find a curated list of articles that dive deeper into each of these areas, offering practical guidance you can apply today.
How Poor Food Absorption Links to Common Gastrointestinal Disorders
- Elliot Grove
- on Oct 14 2025
- 19 Comments