Efavirenz Heart Health: What You Need to Know
When talking about Efavirenz, a non‑nucleoside reverse transcriptase inhibitor commonly prescribed for HIV treatment. Also known as Sustiva, it has been linked to changes in cardiac rhythm, lipid levels, and blood pressure. If you’re on this medication, understanding its link to your heart is crucial. Studies show that efavirenz can modestly raise LDL cholesterol and, in some cases, trigger QT‑interval prolongation. Those effects don’t happen in isolation – they intersect with the broader health picture of someone living with HIV.
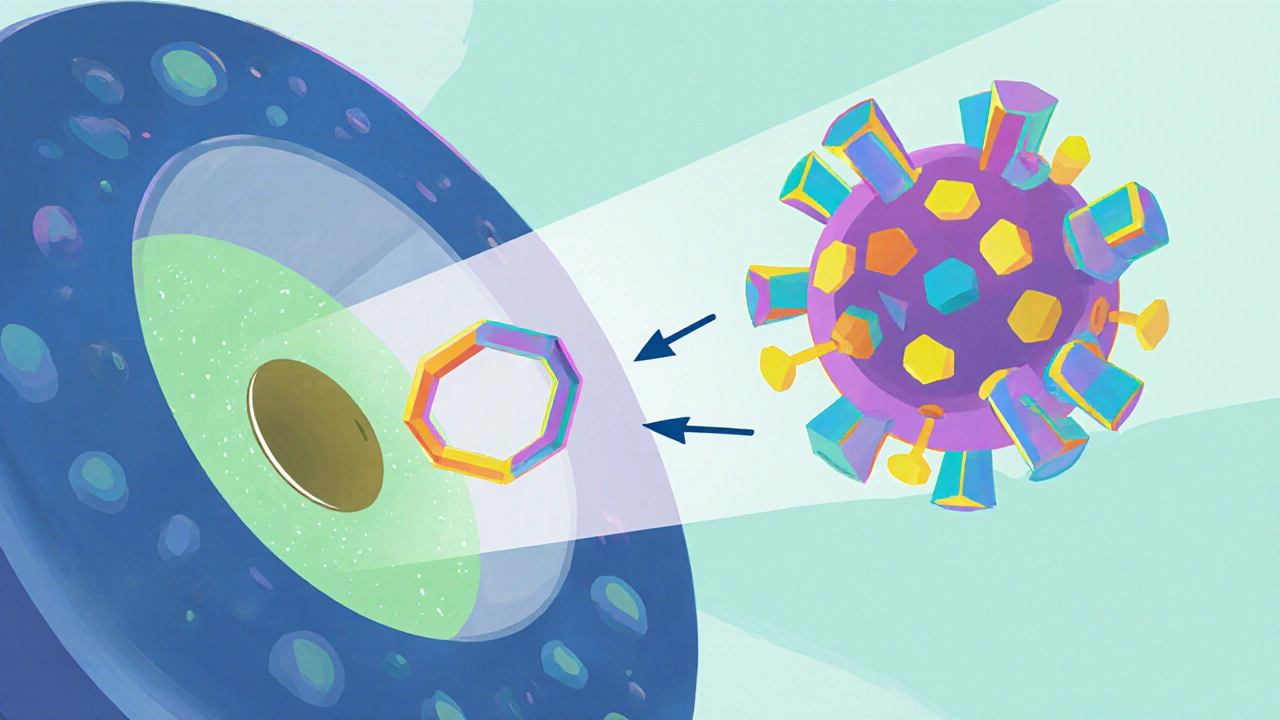
The broader context starts with HIV infection, a chronic viral condition that itself raises inflammation and cardiovascular strain. This inflammation often accelerates atherosclerosis, making cardiovascular disease, including coronary artery disease, arrhythmias, and hypertension. Managing these risks requires a solid antiretroviral therapy, a regimen that keeps viral load low while balancing side‑effect profiles. The therapeutic goal is simple: suppress the virus without compromising the heart. That’s why clinicians monitor lipid panels, ECGs, and blood pressure regularly when efavirenz is part of the regimen. In practice, the relationship can be expressed as three semantic triples:
- Efavirenz can affect heart health.
- HIV infection influences cardiovascular risk.
- Antiretroviral therapy requires cardiac monitoring.
Key Topics in Efavirenz and Cardiac Care
Beyond the drug itself, several heart‑related conditions often appear in the conversation. Efavirenz heart health concerns include atrial fibrillation, especially in pregnant patients where hormone shifts already stress the heart. Our guide on atrial fibrillation in pregnancy details symptoms, risks, and management steps from diagnosis to postpartum care.
Beta‑blockers like Metoprolol are another piece of the puzzle. Metoprolol’s impact on cardiac rehabilitation shows how a well‑chosen medication can offset efavirenz‑induced tachycardia or hypertension. If you’re juggling efavirenz with a beta‑blocker, dose timing and side‑effect vigilance become essential.
Sleep apnea is a hidden driver of coronary artery disease and arrhythmias. Our article on coronary artery disease and sleep apnea explains how untreated apnea can worsen lipid abnormalities already seen with efavirenz. Addressing sleep quality, using CPAP, and lifestyle changes can therefore protect the heart.
For people dealing with supraventricular tachycardia (SVT), driving safety tips are crucial. The SVT driving guide outlines legal requirements and practical strategies to stay safe behind the wheel while managing medication‑induced rhythm changes.
All these topics share a common thread: the need for proactive monitoring and tailored interventions. Whether it’s checking QT intervals, adjusting antiretroviral combos, or adding a beta‑blocker, the goal is to keep the heart stable while the virus stays suppressed.
Below you’ll find a curated collection of articles that dive deeper into each of these areas—arrhythmia management, medication interactions, lifestyle tweaks, and clinical guidelines. Use them as a roadmap to navigate the intersection of efavirenz therapy and heart health, and to make informed decisions with your healthcare team.
Efavirenz and Heart Health: Key Risks and What to Watch For
- Elliot Grove
- on Oct 16 2025
- 14 Comments