Efavirenz QT Interval Risk Calculator
Assess Your QT Interval Risk
Estimate potential QTc prolongation from efavirenz treatment. This tool helps determine if you need additional monitoring or adjustments to your treatment plan.
Efavirenz is a non‑nucleoside reverse transcriptase inhibitor (NNRTI) used in combination antiretroviral therapy (ART) for people living with HIV. While it has helped millions suppress viral load, a growing body of data shows it can nudge the heart in an unwanted direction. This article untangles the science, points out who should be extra careful, and offers practical steps to keep the heart beating strong while staying on treatment.
Understanding Efavirenz: How It Fights HIV
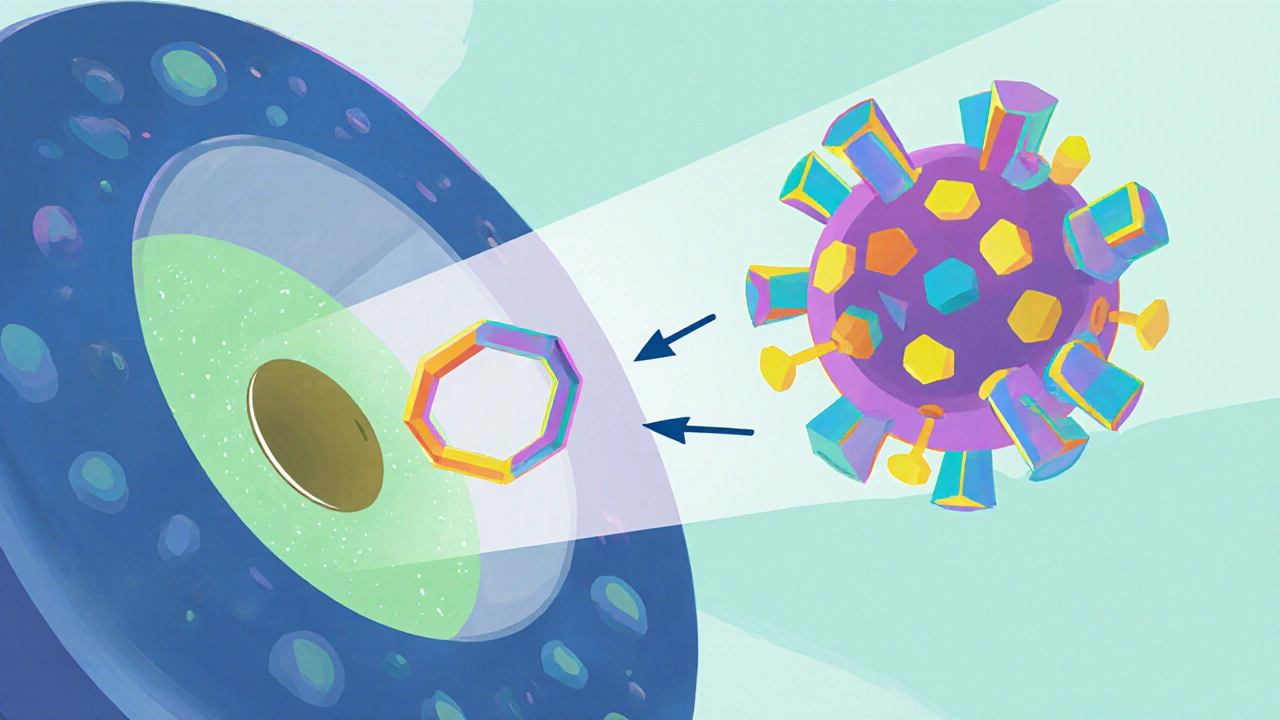
Efavirenz blocks the enzyme reverse transcriptase, stopping the virus from turning its RNA into DNA. Most regimens pair it with two nucleoside reverse transcriptase inhibitors (NRTIs) such as tenofovir and emtricitabine. The standard adult dose is 600mg once daily, taken on an empty stomach to maximize absorption. Because it penetrates the central nervous system well, it also reduces HIV reservoirs in brain tissue.
Cardiovascular Disease in the Context of HIV
Cardiovascular disease (CVD) refers to conditions that affect the heart and blood vessels, including coronary artery disease, stroke, and peripheral artery disease. People living with HIV face a higher CVD risk than the general population-about 1.5‑2 times higher-due to chronic inflammation, lifestyle factors, and some antiretroviral agents.
What the Research Says About Efavirenz and the Heart
Large cohort studies from the United States and Europe have consistently flagged efavirenz as an outlier among NNRTIs when it comes to heart health. A 2022 analysis of 12,000 patients on first‑line ART found a 23% higher incidence of myocardial infarction among those taking efavirenz compared with those on integrase inhibitors. Another meta‑analysis pooled data from ten randomized trials and reported a modest but significant increase in total cholesterol and low‑density lipoprotein (LDL) levels after six months of efavirenz therapy.
Beyond lipids, efavirenz can prolong the QT interval on an electrocardiogram. A prospective study of 320 patients recorded an average QTc increase of 12ms after three months of treatment, raising concerns for arrhythmia in patients with pre‑existing cardiac conduction issues.
Why Efavirenz Affects the Cardiovascular System
Two main pathways explain the link:
- Lipid alteration: Efavirenz interferes with hepatic lipid metabolism, boosting triglycerides and LDL while lowering high‑density lipoprotein (HDL). Over time, these changes accelerate atherosclerotic plaque buildup.
- Direct electrophysiological effect: The drug blocks the hERG potassium channel, which governs the repolarization phase of the cardiac action potential. In susceptible individuals, this action delays ventricular repolarization, manifesting as QTc prolongation.
Genetic variation in the enzyme CYP2B6 also matters. People who are rapid metabolizers clear efavirenz quickly, leading to lower plasma levels and potentially fewer cardiac side effects. Conversely, slow metabolizers experience higher drug exposure, amplifying lipid disturbances and QT changes.
Who Is Most at Risk?
The risk isn’t uniform. Certain groups should be extra vigilant:
- Older adults (≥50years): Age‑related vascular stiffening makes any additional lipid shift more consequential.
- Patients with baseline hypertension or dyslipidemia: Efavirenz can push already borderline numbers over the line.
- Individuals with a family history of sudden cardiac death: QT prolongation becomes a red flag.
- Those on concurrent QT‑prolonging medications: Anti‑psychotics, certain antibiotics, or anti‑emetics can compound the effect.
Screening for these factors before initiating therapy helps clinicians weigh benefits against cardiac risks.
Managing the Cardiovascular Risk While Staying on Efavirenz
Switching to an integrase strand transfer inhibitor (INSTI) is the cleanest solution, but not everyone can change regimens due to resistance patterns or drug interactions. When efavirenz remains the best option, the following strategies keep the heart safe:
- Baseline assessment: Order a fasting lipid panel, blood pressure measurement, and a 12‑lead ECG to capture QTc baseline.
- Follow‑up monitoring: Re‑check lipids and ECG at three months, then every six months. Any QTc >460ms (men) or >470ms (women) warrants a cardiology consult.
- Lifestyle intervention: Encourage a Mediterranean‑style diet, regular aerobic exercise (150minutes per week), and smoking cessation. These actions blunt lipid spikes and improve endothelial function.
- Pharmacologic lipid control: If LDL stays above 130mg/dL after three months, consider adding a statin (e.g., pravastatin, which has minimal interaction with efavirenz).
- Medication review: Avoid adding other QT‑prolonging drugs unless absolutely necessary. If a co‑prescription is unavoidable, increase ECG surveillance.
Quick Reference Checklist for Clinicians
| Step | Action | Timing |
|---|---|---|
| 1 | Obtain fasting lipid panel, blood pressure, and 12‑lead ECG | Before starting efavirenz |
| 2 | Review patient’s cardiovascular history and medication list | Initial visit |
| 3 | Repeat lipid panel and ECG | 3months after initiation |
| 4 | Assess need for statin or lifestyle referral | If LDL>130mg/dL or significant QTc change |
| 5 | Continued monitoring | Every 6months thereafter |

Real‑World Example
Michael, a 52‑year‑old man with well‑controlled HIV, started efavirenz three years ago. His baseline LDL was 110mg/dL, and his QTc measured 425ms. At the 6‑month check, LDL rose to 152mg/dL and QTc reached 448ms. His clinician added pravastatin, advised a low‑saturated‑fat diet, and scheduled an ECG repeat in three months. Six months later, LDL fell to 124mg/dL and QTc stabilized at 432ms. Michael stayed on efavirenz, but the proactive steps prevented a potential heart event.
Bottom Line: Balancing Efficacy and Safety
Efavirenz remains a cornerstone of first‑line ART in many low‑resource settings because of its low cost and high barrier to resistance. However, clinicians must recognize its modest but real impact on heart health. By screening, monitoring, and intervening early, patients can reap the antiviral benefits without compromising cardiovascular well‑being.
Frequently Asked Questions
Does efavirenz cause heart attacks?
Large observational studies show a modest increase in heart‑attack risk-about 20‑30% higher compared with some newer drug classes. The absolute risk remains low, especially in younger patients without other risk factors.
Should I get an ECG before starting efavirenz?
Yes. A baseline ECG helps identify pre‑existing QT prolongation. If the QTc is already near the upper normal limit, a non‑QT‑affecting regimen may be safer.
Can lifestyle changes offset efavirenz‑related lipid spikes?
Yes. A diet rich in omega‑3 fatty acids, regular aerobic exercise, and weight control can lower LDL and triglycerides, often reducing the need for statins.
Is there a genetic test for CYP2B6 that predicts efavirenz side effects?
Pharmacogenetic testing for CYP2B6 variants exists, but it isn’t routinely covered by insurance in most countries. If available, it can help decide dosing or an alternative regimen.
What alternatives have lower cardiovascular risk?
Integrase strand transfer inhibitors such as dolutegravir or bictegravir have a neutral or even beneficial effect on lipid profiles and do not prolong the QT interval, making them preferred when cardiovascular safety is a priority.