Diagnosing Malabsorption: What You Need to Know
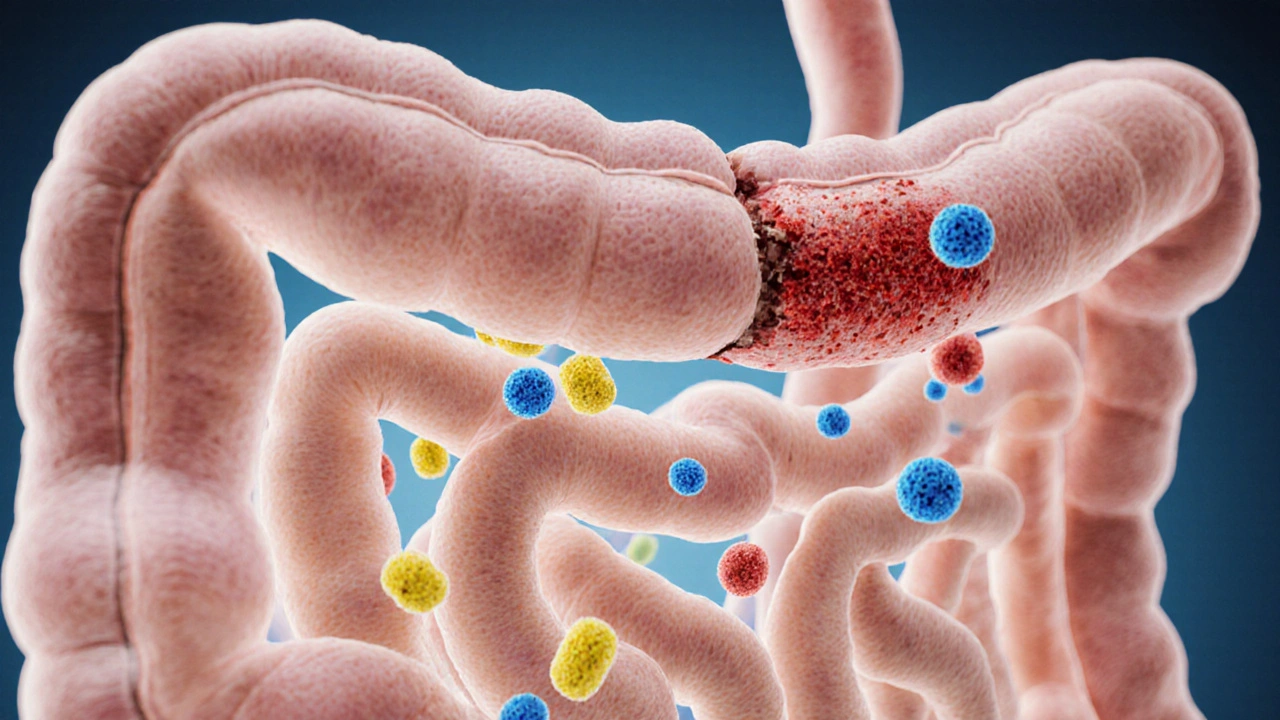
When tackling diagnosing malabsorption, the process of identifying why the body isn’t absorbing nutrients properly. Also known as malabsorption assessment, it requires a mix of symptom review, lab work, and imaging to pinpoint the problem.
One of the first tools doctors reach for is stool analysis, a lab test that checks for fat, blood, and bacterial imbalances. This test can reveal whether undigested fat is slipping through, a classic sign of poor absorption. Alongside stool checks, a breath test, often used to detect bacterial overgrowth or lactose intolerance, offers a non‑invasive way to see how the gut processes sugars and carbs.
How Imaging Complements Lab Tests
When lab results raise flags, doctors often turn to endoscopy, a visual exam of the upper GI tract that can spot inflammation, celiac disease, or structural issues. Endoscopy not only lets physicians take biopsies for microscopic analysis but also helps rule out other gastrointestinal disorders that could mimic malabsorption symptoms. Together, stool analysis, breath tests, and endoscopy create a comprehensive picture, allowing clinicians to pinpoint the exact cause of nutrient loss.
Understanding the relationship between these tools is key: diagnosing malabsorption involves gathering data from biochemical tests, interpreting breath patterns, and visualizing tissue health. Each test informs the next step—if stool analysis shows excess fat, a breath test can check for bacterial overgrowth; if both point to a problem, endoscopy can confirm structural damage. This step‑by‑step approach ensures that treatment targets the real issue, whether it’s enzyme deficiency, celiac disease, or an infection.
Beyond the tests, it’s helpful to know the common culprits. Enzyme deficiencies, such as low pancreatic lipase, prevent fat breakdown. Celiac disease triggers an immune response that flattens the villi in the small intestine, hampering nutrient uptake. Small intestinal bacterial overgrowth (SIBO) interferes with carbohydrate processing, often detected via breath testing. Recognizing these patterns lets patients and clinicians choose the right therapy—diet changes, enzyme supplements, or antibiotics.
Now that you’ve got a sense of the main diagnostic pathways, you’ll see a range of articles below covering each test in depth, practical tips for preparing for appointments, and what to expect after results. Whether you’re facing vague tummy troubles or a known condition, the resources ahead will guide you through every step of the malabsorption puzzle.
How Poor Food Absorption Links to Common Gastrointestinal Disorders
- Elliot Grove
- on Oct 14 2025
- 19 Comments