If you’ve been struggling with persistent redness, bumps, or burning on your face, you’ve probably heard of Soolantra. It’s one of the few FDA-approved treatments specifically for rosacea that targets the underlying cause-not just the symptoms. But it’s not cheap, and it’s not the only option. So how does Soolantra (ivermectin) stack up against other treatments? And more importantly, which one actually works for your skin?
What Soolantra Actually Does
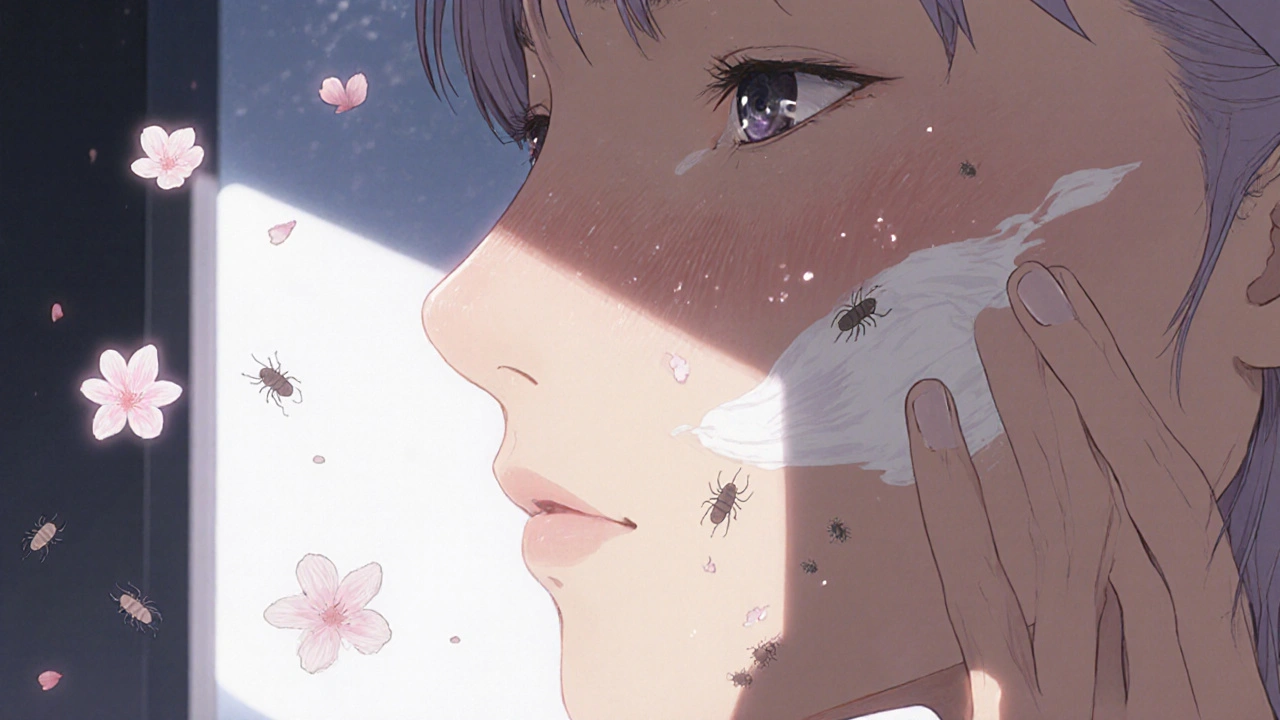
Soolantra is a 1% topical cream with ivermectin as its active ingredient. Unlike antibiotics or steroids, it doesn’t just kill bacteria or calm inflammation. It targets Demodex mites, tiny creatures that live in your hair follicles. For most people, these mites are harmless. But in rosacea patients, they multiply out of control, triggering inflammation, redness, and pimple-like bumps.
Clinical trials showed that after 12 weeks of daily use, over 40% of users saw at least a 90% reduction in inflammatory lesions. That’s not just a little better-it’s a game-changer for people who’ve tried everything else. The cream is applied once a day, usually at night, and most people notice improvement within 2 to 4 weeks. But it’s not instant. You need to stick with it.
Top Alternatives to Soolantra
There are several other prescription and over-the-counter options for rosacea. Here are the most common ones, ranked by effectiveness and practicality.
1. Metronidazole (MetroGel, Noritate)
Metronidazole has been the go-to rosacea treatment for decades. It’s available as a gel, cream, or lotion, and it’s usually cheaper than Soolantra. It works by reducing inflammation and killing bacteria on the skin.
But here’s the catch: it doesn’t touch Demodex mites. That means if your rosacea is mite-driven (and for many, it is), metronidazole won’t fix the root problem. Studies show it reduces lesions by about 30-50% over 9-12 weeks-slower and less complete than Soolantra.
Best for: Mild rosacea, budget-conscious users, or as a maintenance treatment after Soolantra.
2. Azelaic Acid (Finacea, Skinoren)
Azelaic acid is a naturally occurring compound found in grains. In prescription strength (15% gel), it reduces redness, kills bacteria, and gently exfoliates. It’s also safe to use during pregnancy, which makes it a favorite for women.
It works well for both papulopustular rosacea and skin texture issues. One study found 60% of users saw significant improvement after 15 weeks. But it can cause stinging, dryness, or peeling, especially at first. And it takes longer to show results-often 6 to 8 weeks.
Best for: People with sensitive skin, those who want to treat both redness and texture, or anyone avoiding steroids.
3. Brimonidine (Mirvaso)
This one’s different. Brimonidine doesn’t treat bumps or mites. It’s a vasoconstrictor-it shrinks blood vessels to reduce redness. Think of it like a temporary fix. You apply it in the morning, and your face looks less flushed within 30 minutes.
The problem? The effect lasts only 8-12 hours. And if you stop using it, your redness can rebound worse than before. Some users report flushing, burning, or even worsening redness over time. It’s not a cure. It’s a cosmetic cover-up.
Best for: People who need quick redness relief for events or photos, but not as a long-term solution.
4. Oxymetazoline (Rhofade)
Similar to brimonidine, oxymetazoline is a topical vasoconstrictor. It reduces redness for up to 12 hours. It’s slightly less likely to cause rebound flushing than brimonidine, but it still doesn’t treat the underlying cause.
It’s also more expensive than metronidazole and doesn’t help with bumps or pustules. If your main issue is constant flushing, this might be worth a try. But if you have bumps, cysts, or thickened skin, skip it.
5. Oral Antibiotics (Doxycycline, Minocycline)
Oral antibiotics like low-dose doxycycline (40mg modified-release) are often prescribed for moderate to severe rosacea. They reduce inflammation systemically and can be very effective.
But long-term antibiotic use risks gut health, yeast overgrowth, and antibiotic resistance. Many dermatologists now prefer topical treatments like Soolantra to avoid these side effects. Antibiotics are usually a short-term bridge-not a solution.
Comparison Table: Soolantra vs Alternatives
| Treatment | Active Ingredient | Targets Demodex Mites? | Reduces Redness? | Reduces Bumps? | Time to See Results | Typical Cost (30-day supply) |
|---|---|---|---|---|---|---|
| Soolantra | Ivermectin 1% | Yes | Yes | Yes | 2-4 weeks | $300-$450 |
| Metronidazole | Metronidazole | No | Mild | Yes | 6-12 weeks | $50-$100 |
| Azelaic Acid | Azelaic acid 15% | No | Yes | Yes | 6-8 weeks | $150-$250 |
| Brimonidine | Brimonidine tartrate | No | Yes (temporary) | No | 30 minutes | $200-$350 |
| Oxymetazoline | Oxymetazoline hydrochloride | No | Yes (temporary) | No | 15-30 minutes | $250-$400 |
| Oral Doxycycline | Doxycycline 40mg | No | Yes | Yes | 4-8 weeks | $20-$60 |
Who Should Use Soolantra?
If you have moderate to severe papulopustular rosacea-with lots of bumps, pustules, and persistent redness-Soolantra is your best bet. It’s the only topical treatment that directly attacks the Demodex mite population. Studies show it outperforms metronidazole and azelaic acid in lesion reduction.
It’s also ideal if you’ve tried other treatments and they didn’t stick. Many patients switch to Soolantra after antibiotics failed or after redness returned with rebound flushing from brimonidine.
It’s not perfect. It’s expensive. Insurance doesn’t always cover it. And you still need to avoid triggers: spicy food, alcohol, hot showers, and sun exposure. But if your goal is long-term control-not just a quick fix-Soolantra delivers.
Who Should Skip Soolantra?
Don’t start with Soolantra if:
- Your rosacea is mostly redness with few bumps-try brimonidine or oxymetazoline first.
- You’re on a tight budget and need the cheapest option-metronidazole is effective enough for mild cases.
- You’re pregnant or nursing-azelaic acid is safer.
- You’ve had allergic reactions to ivermectin in the past (rare, but possible).
Also, don’t expect miracles if you’re not changing your skincare routine. Harsh cleansers, alcohol-based toners, and physical scrubs will undo any treatment. Gentle, fragrance-free products are non-negotiable.
Combination Therapy: The Real Secret
The most successful rosacea patients don’t rely on just one treatment. They stack them smartly.
For example:
- Use Soolantra at night to kill mites and reduce bumps.
- Apply azelaic acid in the morning to calm redness and improve texture.
- Use sunscreen with zinc oxide daily-sun exposure is the #1 trigger.
- On days when redness flares, use brimonidine for a quick visual reset.
This approach isn’t about using everything at once. It’s about matching the right tool to the right symptom. Soolantra handles the root cause. Other treatments handle the fallout.

What About Natural Remedies?
You’ll see ads for tea tree oil, aloe vera, or green tea extracts as "natural rosacea cures." Some people swear by them. But here’s the truth: there’s no solid clinical evidence that any natural remedy reduces Demodex mites or reliably clears rosacea.
Tea tree oil, for example, has some anti-mite properties in lab studies. But applying it directly to your face can cause severe irritation. Even diluted, it’s not reliable or safe for daily use.
Don’t replace proven treatments with untested oils. Use them only as a supplement-if at all-and always patch test first.
Final Thoughts: What’s the Best Choice?
Soolantra isn’t the cheapest. It’s not the fastest. But it’s the only topical treatment that actually fixes the biological driver of your rosacea. If you’ve tried everything else and still have bumps or persistent redness, it’s worth the investment.
For mild cases, metronidazole or azelaic acid may be enough. For pure redness, brimonidine or oxymetazoline can help-but only temporarily. And oral antibiotics? Use them sparingly.
The goal isn’t to find the best drug. It’s to find the best plan for your skin. That might mean Soolantra alone. Or Soolantra plus azelaic acid plus sunscreen. Or even a short course of antibiotics followed by Soolantra for maintenance.
Work with your dermatologist. Track your triggers. Be patient. Rosacea isn’t cured overnight. But with the right approach, it can be controlled-for years.
Is Soolantra better than metronidazole for rosacea?
Yes, for moderate to severe rosacea with bumps and pustules. Soolantra targets Demodex mites, the root cause, while metronidazole only reduces inflammation and kills surface bacteria. Studies show Soolantra clears lesions faster and more completely than metronidazole.
Can I use Soolantra and azelaic acid together?
Yes, many dermatologists recommend using them together. Apply Soolantra at night to target mites, and azelaic acid in the morning to reduce redness and improve skin texture. Just wait 15-20 minutes between products to avoid irritation.
Does Soolantra cause skin dryness or peeling?
Soolantra is generally well-tolerated. Unlike retinoids or azelaic acid, it rarely causes dryness or peeling. Some users report mild stinging or burning at first, but that usually fades within a week. If irritation persists, talk to your doctor.
How long should I use Soolantra before seeing results?
Most people notice improvement in 2 to 4 weeks. Full results typically take 12 weeks of daily use. Don’t stop early-even if you see progress. Stopping too soon can lead to a rebound flare.
Is Soolantra safe for long-term use?
Yes. Clinical studies have shown Soolantra is safe for use over 40 weeks and beyond. Unlike antibiotics, it doesn’t cause resistance or gut issues. Many patients use it indefinitely as a maintenance treatment to prevent flare-ups.
Can I use Soolantra if I have sensitive skin?
Soolantra is formulated for sensitive skin and doesn’t contain alcohol, fragrances, or harsh preservatives. If you’ve had reactions to other topical treatments, Soolantra is often a better choice. Still, patch test it on a small area first.
Next Steps
Start by identifying your main symptoms: Is it redness? Bumps? Burning? Then match your treatment to the cause. If you’re unsure, ask your dermatologist for a skin scraping test to check for Demodex mites. That simple test can tell you whether Soolantra is your best option.
Don’t settle for temporary fixes. Rosacea is chronic, but it’s not hopeless. With the right treatment plan, you can get back to feeling confident in your skin-without hiding behind makeup or avoiding social events.