Sodium Intake Calculator
Daily Sodium Tracker
Estimate your sodium intake from food and see how it affects blood pressure medication effectiveness. Recommended daily limit: 1,500 mg (ideal) or 2,300 mg (maximum).
Your Results
Your sodium intake is 0 mg. This is below recommended limits.
According to the JAMA study, reducing sodium by about 1 teaspoon (2,300 mg) lowered systolic blood pressure by 6 mm Hg — equivalent to starting a first-line blood pressure pill.
Why this matters for your meds:
- High sodium makes blood pressure medications less effective
- Reduction in sodium could help your medication work better
- Measurable drops in blood pressure can happen within 7 days of sodium reduction
When you're taking medication for high blood pressure, your salt intake might be silently undoing all the hard work your pills are doing. It’s not just about avoiding the salt shaker - it’s about understanding how the sodium hiding in your bread, soup, and frozen meals is making your meds less effective. A 2023 study published in JAMA found that cutting daily sodium intake by about one teaspoon (2,300 mg) lowered systolic blood pressure by 6 mm Hg - the same drop you’d get from starting a first-line blood pressure pill like an ACE inhibitor. And here’s the kicker: this worked for 70-75% of people, even those already on medication.
Why Salt Makes Your Blood Pressure Meds Work Less
Your blood pressure medications don’t operate in a vacuum. They rely on your body’s fluid balance, blood vessel tone, and kidney function to do their job. Too much sodium throws all of that off. Sodium pulls water into your bloodstream, increasing your blood volume. That extra fluid pushes harder against your artery walls - raising your pressure. Medications like diuretics, ACE inhibitors, and ARBs are designed to counteract this. But when you keep flooding your system with salt, they’re fighting a losing battle. For example, diuretics help your body flush out extra fluid. But if you’re eating 4,500 mg of sodium a day - the average for many Americans - your kidneys can’t keep up. The diuretic might help a little, but the salt keeps pulling water back in. ACE inhibitors and ARBs work by relaxing blood vessels. But high sodium stiffens those vessels and reduces the drugs’ ability to widen them. The result? Your numbers stay stubbornly high, even if you’re taking your pills exactly as prescribed.How Much Salt Are You Really Eating?
Most people think they’re cutting back because they stop adding salt to their food. But here’s the truth: 70% of the sodium you consume comes from packaged, processed, and restaurant foods. That means your breakfast cereal, canned beans, deli meat, pasta sauce, and even your favorite “healthy” granola bar could be loaded with salt. A single slice of store-bought bread can have 230 mg of sodium. Two slices? That’s 10% of your daily limit before you even eat lunch. A typical frozen lasagna? Often over 1,200 mg. A small bowl of soup? Could be 800 mg. Add a sandwich with deli turkey and cheese, and you’re already at 2,000 mg by midday. The American Heart Association recommends no more than 2,300 mg per day - and ideally, 1,500 mg. Yet most people eat 3,400 mg or more. That’s not just “a little extra.” That’s enough to cancel out the effect of your medication.What Happens When You Cut Back - Fast
You don’t need to wait months to see results. In the 2023 JAMA study, participants saw measurable drops in blood pressure within just seven days of switching to a low-sodium diet (500 mg per day). That’s faster than many medications take to kick in. The study tracked 213 adults, mostly over 60, with a mix of those on blood pressure meds and those who weren’t. When they ate their usual diet (around 4,500 mg sodium), their average systolic blood pressure was 125 mm Hg. When they cut back to 500 mg, it dropped to 119 mm Hg. That 6-point drop isn’t just a number - it’s the difference between a moderate risk of stroke and a much lower one. And it’s not just about the number on the monitor. High sodium also increases protein in your urine - a sign your kidneys are under stress. Blood pressure medications like ACE inhibitors are often prescribed to protect your kidneys, especially if you have diabetes. But if you keep eating salty food, those meds can’t do their job properly. Reducing sodium helps them work better, and your kidneys thank you.
Who Benefits the Most?
Not everyone responds the same way to sodium reduction. About 25-30% of people are “non-responsive” - their blood pressure barely budges when they cut salt. But that doesn’t mean it’s pointless for them. For the rest - the majority - the effect is powerful. People who benefit most include:- Those over 50
- People with existing high blood pressure
- Black individuals (who tend to be more salt-sensitive)
- People with diabetes or kidney disease
- Those taking diuretics, ACE inhibitors, or ARBs
How to Actually Reduce Sodium - Without Giving Up Food
You don’t need to eat bland food or starve yourself. You just need to know where the salt hides - and how to outsmart it. Read labels like a detective. Look at the “Sodium” line in milligrams (mg), not the % Daily Value. Anything under 140 mg per serving is considered low. Avoid anything with more than 400 mg per serving unless it’s a meal you’re eating once a week. Choose fresh or frozen without sauce. Fresh vegetables, chicken, fish, and plain frozen veggies are your friends. Avoid anything with “seasoned,” “marinated,” “broth-based,” or “flavored.” Swap salt for herbs and spices. Garlic powder, onion powder, smoked paprika, cumin, lemon zest, and black pepper add flavor without sodium. Try a salt-free seasoning blend - many are now available in grocery stores. Be smart with condiments. Soy sauce, ketchup, salad dressing, and even some “low-fat” yogurts are sodium bombs. Look for “no salt added” versions. A tablespoon of regular soy sauce has 1,000 mg. The low-sodium version? Around 600 mg - still high, but better. Don’t rely on salt substitutes blindly. Potassium chloride substitutes can be helpful - but not if you have kidney disease. Talk to your doctor before switching. Too much potassium can be dangerous if your kidneys can’t clear it.What About Your Medication Dose?
This is where things get exciting. If you cut sodium and your blood pressure drops, your doctor might be able to lower your medication dose. Fewer pills, fewer side effects, less cost - and just as good control. In the JAMA study, the 6 mm Hg drop from sodium reduction was equivalent to half the effect of starting a new blood pressure pill. That means if you’re on a low dose of lisinopril or losartan, cutting salt could get you to your target without needing to increase the dose. Some patients have even been able to stop one medication entirely after switching to a low-sodium diet and improving other habits like exercise and sleep. It’s not magic - it’s science.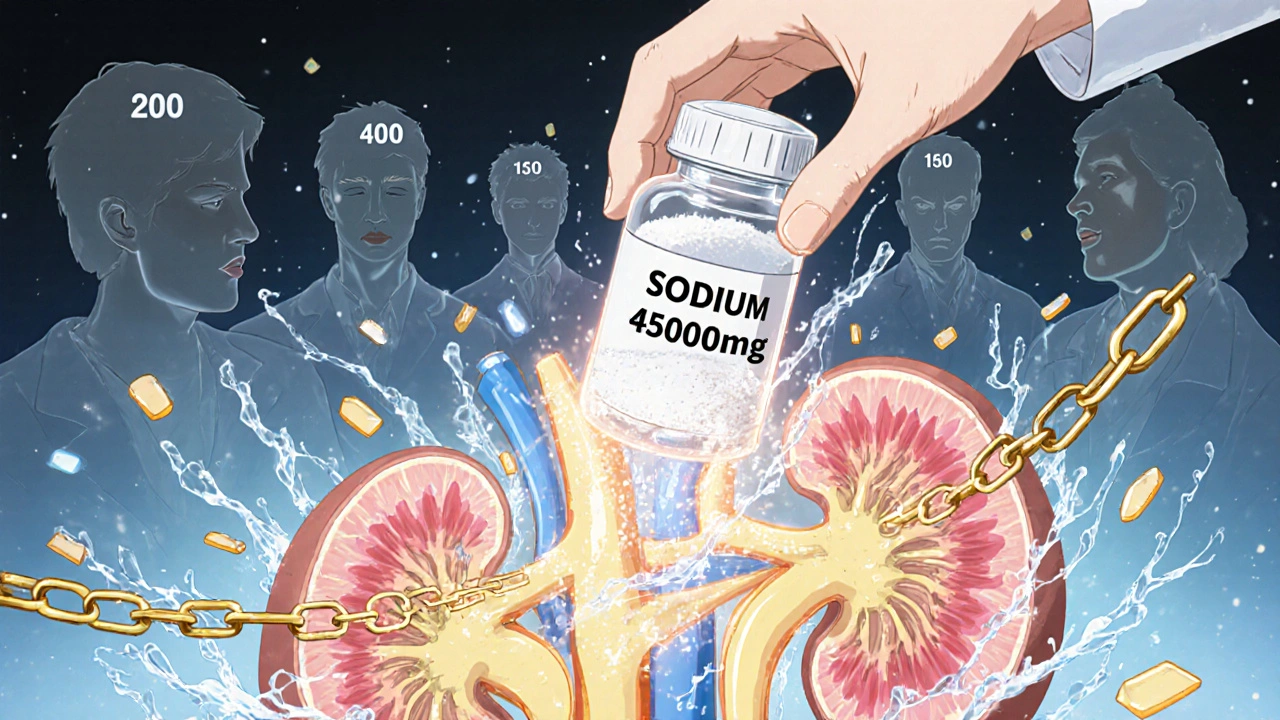
What’s Holding People Back?
The biggest barrier isn’t willpower - it’s confusion. People don’t know what’s high in sodium. They think they’re eating healthy because they avoid sugar or fat. But sodium is sneaky. Another issue? Doctors don’t always talk about it. A 2023 AMA survey found that only 41% of patients with hypertension received clear guidance on sodium limits from their provider. That’s a gap. You need to ask: “Is my salt intake making my meds less effective?” The FDA has set voluntary sodium reduction targets for food manufacturers, aiming to get average intake down to 3,000 mg by 2026. But researchers say that’s still too high. The real goal should be 1,500-2,000 mg - the level linked to the biggest drop in heart attacks and strokes.What’s Next?
Researchers are now building apps to help people track sodium in real time. One tool, being tested in Sydney, Melbourne, and Atlanta, alerts users when their daily sodium intake is climbing too high - and even suggests lower-sodium alternatives based on what they’re eating. It’s not available yet, but it’s coming. For now, the best tool you have is awareness. Start by checking the sodium content of your top five go-to foods. Write them down. Then pick one to swap out this week. Maybe it’s switching from canned soup to homemade broth. Or choosing unsalted nuts instead of salted. Small steps add up.Final Thought: This Isn’t a Diet. It’s a Treatment.
Reducing sodium isn’t about being perfect. It’s about making your medication work better. You wouldn’t skip your blood pressure pill because you felt fine one day. Don’t treat sodium like an optional extra. It’s part of your treatment plan - just as important as the pill in your hand. If you’re on blood pressure meds and your numbers aren’t budging, ask yourself: Am I eating enough salt to cancel out what my pills are trying to do? The answer might be yes. And the fix? It’s on your plate.Can I still eat out if I’m trying to reduce sodium for my blood pressure meds?
Yes, but you need to be strategic. Ask for sauces and dressings on the side, skip the salted sides like fries or pickles, and choose grilled or steamed proteins over fried or breaded options. Many restaurants now list sodium content online - check before you go. Opt for dishes labeled “low sodium” or ask if they can prepare your meal without added salt.
Will cutting salt lower my blood pressure even if I’m already on medication?
Yes. A major 2023 study showed that people already on blood pressure medication saw a 6 mm Hg drop in systolic pressure just by reducing sodium intake - the same effect as starting a new drug. Salt doesn’t just raise blood pressure; it makes your meds less effective. Cutting back helps them work better.
How quickly will I see results after cutting back on salt?
You can see measurable drops in blood pressure within 7 days. The 2023 JAMA study showed participants’ blood pressure fell noticeably after just one week on a low-sodium diet (500 mg per day). This is faster than many medications take to reach full effect.
Are salt substitutes safe to use with blood pressure meds?
Potassium-based salt substitutes can help reduce sodium, but they’re not safe for everyone. If you have kidney disease, diabetes, or are taking certain meds like ACE inhibitors or ARBs, too much potassium can build up in your blood and become dangerous. Always talk to your doctor before switching to a salt substitute.
Does everyone respond to low-sodium diets the same way?
No. About 70-75% of people see a clear drop in blood pressure when they cut sodium. The rest - around 25-30% - are considered “non-responsive.” But even for them, reducing sodium helps protect the heart and kidneys over time. It’s still a smart move, even if the number on the scale doesn’t change much.
Can reducing salt help me take fewer blood pressure pills?
Yes. Many patients who cut sodium significantly are able to reduce their medication dose - or even stop one pill entirely - because their blood pressure improves enough on their own. This isn’t guaranteed, but it’s common enough that doctors are starting to recommend sodium reduction as a first step before increasing medication.
Is it true that most sodium comes from processed food, not the salt shaker?
Yes. About 70% of the sodium in the average diet comes from packaged and restaurant foods - not from adding salt at the table. That means your bread, canned soup, deli meat, frozen meals, and even “healthy” snacks are the real culprits. Checking labels is more important than avoiding the salt shaker.
What’s the ideal daily sodium limit if I’m on blood pressure medication?
The American Heart Association recommends no more than 1,500 mg per day for people with high blood pressure. The absolute maximum is 2,300 mg - but that’s still too high for most people on meds. Striving for 1,500 mg gives you the best chance of getting your blood pressure under control with your current medications.

