When your child gets sick, you want the best care-fast, safe, and effective. Many parents assume that a generic drug is just a cheaper version of the brand-name medicine, and that’s usually true for adults. But for kids? It’s not that simple. Generic drugs for children can carry hidden risks that most people never think about. The active ingredient might be the same, but the fillers, flavors, colors, and even the liquid concentration can make a dangerous difference in a small body.
Why Kids Aren’t Just Small Adults
Children’s bodies don’t process medicine the same way adults do. Their liver and kidneys are still growing. Their stomachs absorb drugs differently. Their brains are more sensitive to certain chemicals. That’s why a drug that’s perfectly safe for a 40-year-old can be risky-or even deadly-for a 2-year-old. Take acetaminophen. In adults, too much can damage the liver. But in very young children, their bodies actually handle it better because they produce more of a protective enzyme called glutathione. That doesn’t mean they can take more-it means the way we dose it has to be precise. Too little won’t help. Too much can still be dangerous, especially if the wrong concentration is used. And then there’s aspirin. It’s banned for kids under 19 because of Reye’s syndrome, a rare but deadly condition that swells the brain and liver. Even if a generic aspirin tablet has the exact same active ingredient as the brand name, it’s still not safe for children. That’s not about the brand-it’s about the drug itself.The Hidden Dangers in Inactive Ingredients
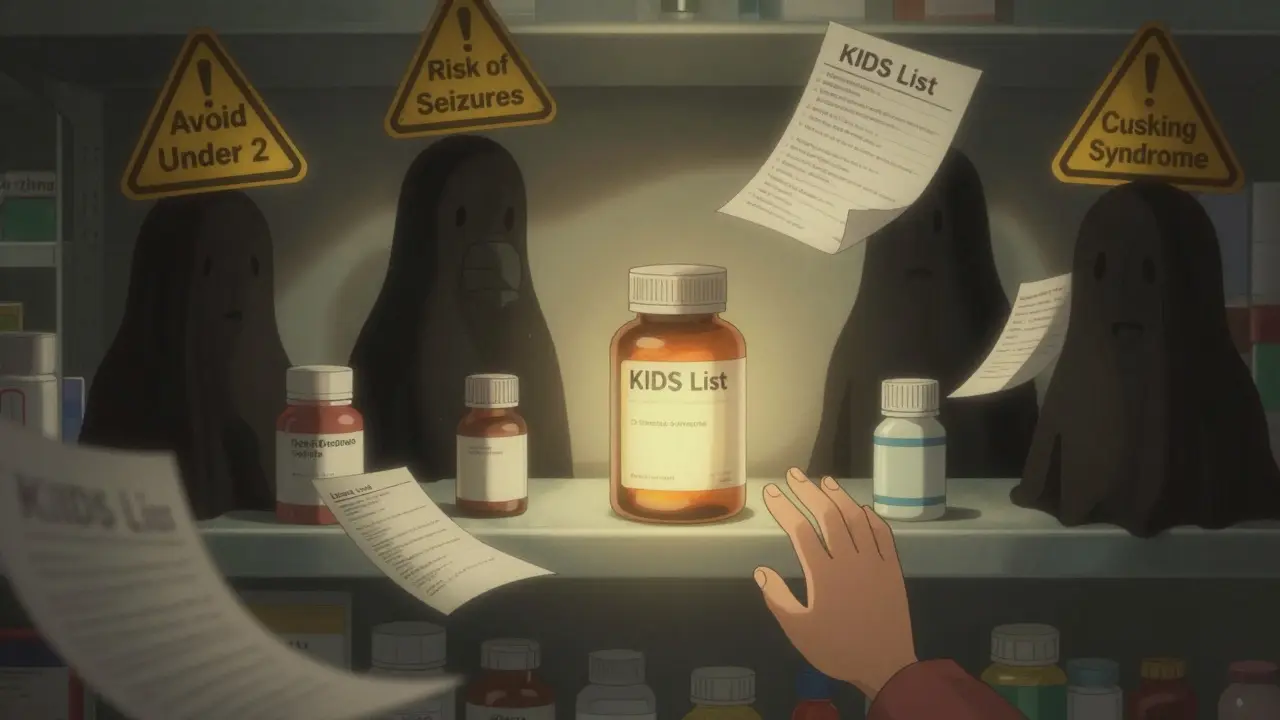
Generic drugs must contain the same active ingredient as the brand name. But they don’t have to use the same fillers, dyes, or preservatives. And for kids, those extras matter a lot. Benzocaine, a common numbing agent in teething gels, can cause methemoglobinemia-a condition where the blood can’t carry oxygen properly. It’s rare, but it’s deadly in babies under 2. The FDA warns against using any product with benzocaine in children under 2. That includes both brand-name and generic versions. But here’s the catch: some generic teething gels have higher concentrations of benzocaine than others. If you switch from one generic to another without checking, you could accidentally double the dose. Lidocaine viscous, used for mouth sores, carries the same warning. One teaspoon too much can cause seizures in a toddler. And because generic versions vary in concentration, parents might think they’re giving the same amount when they’re not. Even colors and flavors can cause problems. A 2024 Reddit thread from over 1,200 parents found that 18% reported allergic reactions after switching to a generic version-mostly because of new dyes or preservatives like propylene glycol or parabens. One mom described her 5-month-old breaking out in hives after switching from brand-name cetirizine to a generic. The doctor said it was “just a different brand.” But the reaction stopped only when they went back to the original.The KIDs List: What Drugs to Avoid
The Pediatric Pharmacy Association created the KIDs List-a living guide of drugs that are risky for kids. It’s not just about brand names. It’s about every version, generic or not. Promethazine, a common antihistamine for nausea or allergies, is on the “avoid” list for kids under 2. Why? It can cause breathing to stop. There have been deaths. Even in older kids, it’s a “caution” drug. But many pharmacies automatically substitute it because it’s cheap and widely available. Trimethobenzamide, an anti-nausea drug, is banned for anyone under 18. It can trigger severe muscle spasms called dystonic reactions. One 16-year-old ended up in the ER after taking a generic version for vomiting. The doctor didn’t know it was on the KIDs List. Topical steroids like betamethasone are used for eczema and diaper rash. But in kids under 2, they can cause Cushing syndrome-where the body makes too much cortisol. This leads to weight gain, high blood pressure, and weakened bones. Generic versions come in different strengths. Some are labeled “high potency.” Others are “medium.” If you grab the wrong one, you’re putting your child at risk. The KIDs List is updated every quarter. In January 2025, 17 new drugs were added, including linaclotide (for constipation) and guaifenesin (for cough). Linaclotide can cause fatal dehydration in kids under 2. Guaifenesin isn’t safe under age 4. Yet these drugs are still sold over the counter as generics.
Off-Label Use: The Silent Problem
About 40% of all pediatric prescriptions are off-label-meaning the drug wasn’t approved for that age, condition, or dose. And 90% of those prescriptions are for generics. Why? Because manufacturers rarely test drugs on kids. It’s expensive. It’s hard to get consent. So doctors guess. They take the adult dose, scale it down by weight, and hope for the best. But scaling doesn’t always work. A child’s metabolism changes every few months. A 10-pound infant isn’t just a 1/10th-sized adult. Their liver can’t break down drugs the same way. That’s why levothyroxine (for hypothyroidism) and phenytoin (for seizures) are so dangerous as generics. Even tiny differences in absorption can lead to under- or over-treatment. One study found that switching generic brands of levothyroxine caused thyroid levels to swing dangerously in 1 in 5 children. And here’s the scary part: most parents don’t know. They assume if the doctor prescribed it, it’s safe. They don’t ask if it’s been studied for kids. They don’t check the label for age restrictions.How to Keep Your Child Safe
There are steps you can take-right now-to protect your child.- Ask: “Is this drug approved for my child’s age?” If the answer is no, ask why and if there’s a safer alternative.
- Check the KIDs List. It’s free online. Type in the drug name and see if it’s flagged for kids.
- Use oral syringes, not spoons. Household spoons vary in size. A teaspoon of medicine could be 3-5 mL off. That’s a 50% error. Oral syringes are accurate to 0.1 mL.
- Never use a zero after a whole number. Write “1” not “1.0.” A doctor’s handwriting can make “1.0” look like “10.” That’s a 10-fold overdose. The American Academy of Pediatrics calls this the “zero rule.”
- Keep a current medication list. Include every pill, drop, cream, and supplement-even herbal ones. Bring it to every appointment.
- Ask if you can “Dispense as Written.” If your child has had a reaction to a generic before, or if the drug is on the KIDs List, tell the pharmacist: “Do not substitute.”