Why Weight Matters More Than Age in Kids’ Medication
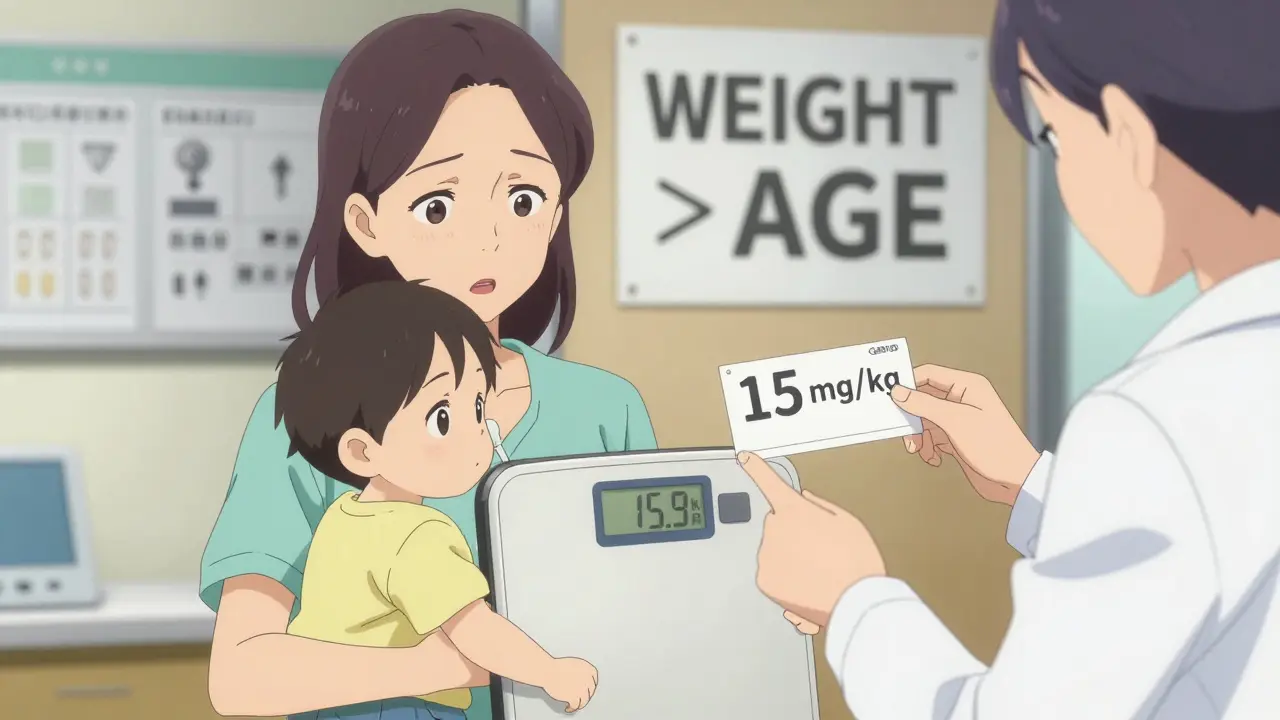
When giving medicine to a child, age doesn’t tell you enough. A 2-year-old could weigh 9 kilograms-or 15. That’s a 67% difference. If you dosed both kids the same because they’re "both 2 years old," one might get too little medicine and the other could get a dangerous overdose. That’s why doctors and nurses don’t use age alone. They use weight.
Every time a child gets a prescription-whether it’s antibiotics, fever reducers, or even pain meds-the first thing the provider checks is weight. Not age. Not height. Not "looks about right." Weight. In kilograms. And that number becomes the foundation for every single dose.
The Math Behind the Dose: mg/kg Explained
Most pediatric medications are dosed in milligrams per kilogram (mg/kg). That means for every kilogram of body weight, the child gets a set number of milligrams of medicine.
Let’s say the order is 15 mg/kg of amoxicillin for an ear infection. The child weighs 16 kg. You multiply: 15 × 16 = 240 mg total per day. If it’s given twice a day, you split it: 120 mg per dose.
It sounds simple. But here’s where things go wrong.
Parents and even some staff mix up pounds and kilograms. In the U.S., scales often show pounds. But every calculation must be in kilograms. The rule is fixed: 1 kg = 2.2 lb. No exceptions.
So if a child weighs 35 pounds, you don’t guess. You divide: 35 ÷ 2.2 = 15.9 kg. Do it wrong-say, you divide by 2-and you’re off by 10%. That’s not a small mistake. That’s a risk of hospitalization.
Concentration Matters Too: It’s Not Just About Milligrams
Not all liquid medicines are the same. Two bottles of acetaminophen might look identical, but one could be 160 mg per 5 mL, and the other 500 mg per 5 mL. That’s more than triple the strength.
Parents often switch between infant and children’s formulas without realizing the concentration changed. A dose that was safe yesterday could be toxic today if the concentration isn’t checked.
Always look at the label. Write down: total dose needed (in mg), concentration (mg/mL), then divide to get volume (mL). For example: need 240 mg, concentration is 160 mg/5 mL. That’s 32 mg per mL. 240 ÷ 32 = 7.5 mL. Use a syringe. Never a spoon.

When Weight Isn’t Enough: BSA and Special Cases
For some drugs-especially chemotherapy, epilepsy meds, or heart medications-weight alone still isn’t precise enough. That’s where body surface area (BSA) comes in.
BSA uses both height and weight. The Mosteller formula is standard: √(height in cm × weight in kg ÷ 3600). A child who is 97 cm tall and weighs 16.8 kg has a BSA of about 0.67 m². The dose is then calculated in mg per m².
Why bother? Because kids with the same weight can have very different body shapes. BSA accounts for that. It’s more complex, but for high-risk drugs, it’s safer.
Some medications also have caps. For example, buprenorphine (used for pain in older kids) is dosed by weight-but capped at 0.4 mg/kg/hour, even if the math says more. That’s because the body can’t safely handle more, no matter how heavy the child is.
The Most Common Mistakes (and How to Avoid Them)
Studies show that 80% of pediatric dosing errors come from unit confusion-mixing up pounds and kilograms. Another 15% come from misreading "mg/kg/d" (which means daily total) instead of "mg/kg/dose" (which means per administration).
Here’s what goes wrong in real life:
- A child weighs 15 kg. Order is 20 mg/kg/day. Parent multiplies 15 × 20 = 300 mg/day. But the order says "20 mg/kg/d"-and the prescriber meant per dose, not per day. Result: child gets 600 mg instead of 300.
- Parent uses a kitchen spoon because they don’t have a syringe. A teaspoon holds 5 mL, but the dose is 7.5 mL. They guess. Overdose.
- They use infant Tylenol (160 mg/5 mL) for a 4-year-old, but the bottle says "for infants under 2." They don’t check concentration. Dose is wrong.
Solutions? Always double-check. Use a syringe. Ask the pharmacist: "Is this the right concentration?" If the order says "mg/kg/d," ask the doctor to clarify: "Do you mean daily total or per dose?"
Tools That Save Lives: Electronic Systems and Double Checks
Hospitals don’t leave this to memory. Most use electronic health records (EHRs) like Epic or Cerner. When you enter a child’s weight in pounds, the system auto-converts to kg. Then it auto-calculates the dose based on the drug’s standard protocol.
And it doesn’t stop there. If the dose is outside safe limits, the system flags it. It might say: "This dose exceeds recommended maximum for weight. Confirm?"
At major children’s hospitals, two licensed staff members must verify high-risk doses before giving them. That’s called a double-check. It’s not optional. It’s policy.
Even then, mistakes happen. That’s why the American Academy of Pediatrics updated its guidelines in 2023 to require dual verification for all "high-alert medications"-drugs like insulin, morphine, and chemotherapy.

What Parents Should Know: Safety Beyond the Numbers
Parents aren’t expected to be pharmacists. But they’re the ones giving the medicine. That means they need to understand three things:
- Weight is king. Always know your child’s weight in kilograms. If you only know pounds, convert it: divide by 2.2.
- Check the label. Concentration changes. Always read the mg/mL or mg/5mL on the bottle.
- Use the right tool. Never use a teaspoon. Use the syringe that came with the medicine.
And if you’re unsure? Call the pediatrician. Don’t guess. Don’t look it up on a website. Call.
Some drugs shouldn’t be given at all to young kids. Benadryl, for example, is not recommended for children under 2 unless a doctor says so. That rule doesn’t change based on weight. Age matters here.
The Bigger Picture: Why This System Exists
Weight-based dosing didn’t come from a textbook. It came from tragedy.
In the 1980s and 90s, too many children died from overdoses because they were given adult doses or age-based estimates. One case in 2021 made headlines: a 15 kg child got 10 times the correct dose of amoxicillin because the nurse misread pounds as kilograms. The child was hospitalized with severe vomiting and dehydration.
That’s why the Institute for Safe Medication Practices says pediatric medication errors happen twice as often as in adults. And why the Joint Commission made pediatric dosing a National Patient Safety Goal.
Today, 98% of U.S. hospitals use weight-based dosing. Community pharmacies? Only 76%. That gap is dangerous. A parent might get a prescription filled at a pharmacy that doesn’t double-check the math.
That’s why you need to be your child’s advocate. Ask: "Did you calculate this based on weight?" "Can you show me how you got this dose?"
Final Rule: When in Doubt, Pause
Medication safety isn’t about being perfect. It’s about being careful.
If the math feels off, stop. If the dose looks too big or too small, question it. If the label doesn’t match what you expected, call the pharmacy. If the doctor wrote "mg/kg/d" without clarifying, ask for the full order.
There’s no shame in asking. There’s only danger in assuming.
Children aren’t small adults. Their bodies process medicine differently. Their weight changes fast. Their safety depends on precision-not guesswork.
Get the weight right. Convert it right. Check the concentration. Use the syringe. Double-check. And when in doubt? Call your provider.
How do I convert my child’s weight from pounds to kilograms?
Divide the weight in pounds by 2.2. For example, if your child weighs 44 pounds, divide 44 by 2.2 to get 20 kg. Never estimate. Always use the exact number on the scale and do the math.
What if the prescription says "mg/kg/d"? Does that mean per day or per dose?
"mg/kg/d" means total daily dose. But many prescribers use unclear shorthand. Always clarify: "Is this the total daily amount, or the amount per dose?" If it’s daily, divide by how many times you give it. For example, 30 mg/kg/day divided into two doses means 15 mg/kg per dose.
Why can’t I just use a teaspoon to give liquid medicine?
A teaspoon holds about 5 mL, but not all teaspoons are the same. Some hold more, some less. Medication syringes are marked in milliliters and are designed for accuracy. Using a spoon can lead to underdosing or overdosing by 20-50%. Always use the syringe that comes with the medicine.
Are there medicines that shouldn’t be given based on age, even if the weight is right?
Yes. For example, Benadryl (diphenhydramine) is not recommended for children under 2 years old unless a doctor specifically says to use it. Some antibiotics, sedatives, and cough medicines also have age restrictions. Weight tells you how much to give-but age can tell you whether you should give it at all.
What should I do if I think I gave the wrong dose?
Call your pediatrician or poison control immediately. Don’t wait for symptoms. In Australia, call Poison Information on 13 11 26. In the U.S., call 1-800-222-1222. Have the medicine bottle handy so you can tell them the name, concentration, and how much was given.