INR Target Range Calculator
Find your target INR range based on your specific medical condition and treatment purpose. Understanding your target range is critical for safe and effective warfarin therapy.
Your Target INR Range
CriticalTarget Range:
This range helps balance clot prevention with bleeding risk.
When you're on a blood thinner like warfarin, your life doesn't revolve around the medication itself-it revolves around a number: your INR. It’s not just a lab result. It’s the difference between staying safe and risking a stroke, or avoiding a dangerous bleed. This number tells your body whether the blood is thin enough to prevent clots but not so thin that it won’t stop bleeding. And getting it right? That’s the daily job of managing your therapy.
What Exactly Is INR?
INR stands for International Normalized Ratio. It’s a standardized way to measure how long it takes your blood to clot. Before INR existed, every lab used different chemicals and methods to test clotting time, so a result of 2.0 in one hospital might mean something completely different in another. That’s dangerous when you’re on a drug like warfarin, where even a small mistake can lead to disaster.
The INR system, developed by the World Health Organization in 1983, fixed that. Now, no matter where you get tested-whether it’s a hospital in Sydney, a clinic in Melbourne, or your own kitchen-the same INR value means the same thing. A result of 2.5 means your blood takes 2.5 times longer to clot than a healthy person’s. That’s the goal: consistency.
For someone not taking blood thinners, a normal INR is 1.0. But if you’re on warfarin, your target isn’t 1.0. It’s higher. Most people need to stay between 2.0 and 3.0. That’s the sweet spot. Below that, clots can form. Above that, you risk bleeding inside your brain, gut, or joints.
Why Does Your Target Change?
Not everyone on warfarin has the same INR goal. Your target depends on what you’re being treated for.
- If you have atrial fibrillation or a blood clot in your leg or lung, your target is usually 2.0-3.0.
- If you have a mechanical mitral valve (a type of heart valve replacement), you need a tighter range: 2.5-3.5.
- For a mechanical aortic valve, it’s still 2.0-3.0, but some doctors may push it higher if you’ve had clots before.
Why the difference? Mechanical valves are rough surfaces inside your heart. Blood is more likely to clot on them. A higher INR keeps that from happening. But higher INR also means higher bleeding risk. So doctors balance the two-clot prevention versus bleeding danger.
Studies show that patients who stay within their target range 70% of the time cut their stroke risk by more than 40%. Those who drift out of range? Their risk of major bleeding goes up by nearly 30% for every 0.5-point increase above 3.0.
How Often Do You Need to Test?
When you first start warfarin, you might test every few days. Your dose is being fine-tuned. Your body reacts differently to food, other meds, even the weather. That’s why early testing is frequent.
Once you’re stable-meaning your INR stays within range for several months-you can cut back. Most people test once a month. But here’s the catch: too many people test too often. A 2021 study found that 38% of stable patients were getting tested weekly, even though there’s no medical reason to. That’s extra finger pricks, extra trips, extra cost.
On the flip side, if your INR jumps above 4.9, you’re in danger. That’s when bleeding becomes likely. If your INR hits 5.0 or higher, you should skip your next warfarin dose and call your doctor immediately. Don’t wait. Don’t guess. Call.

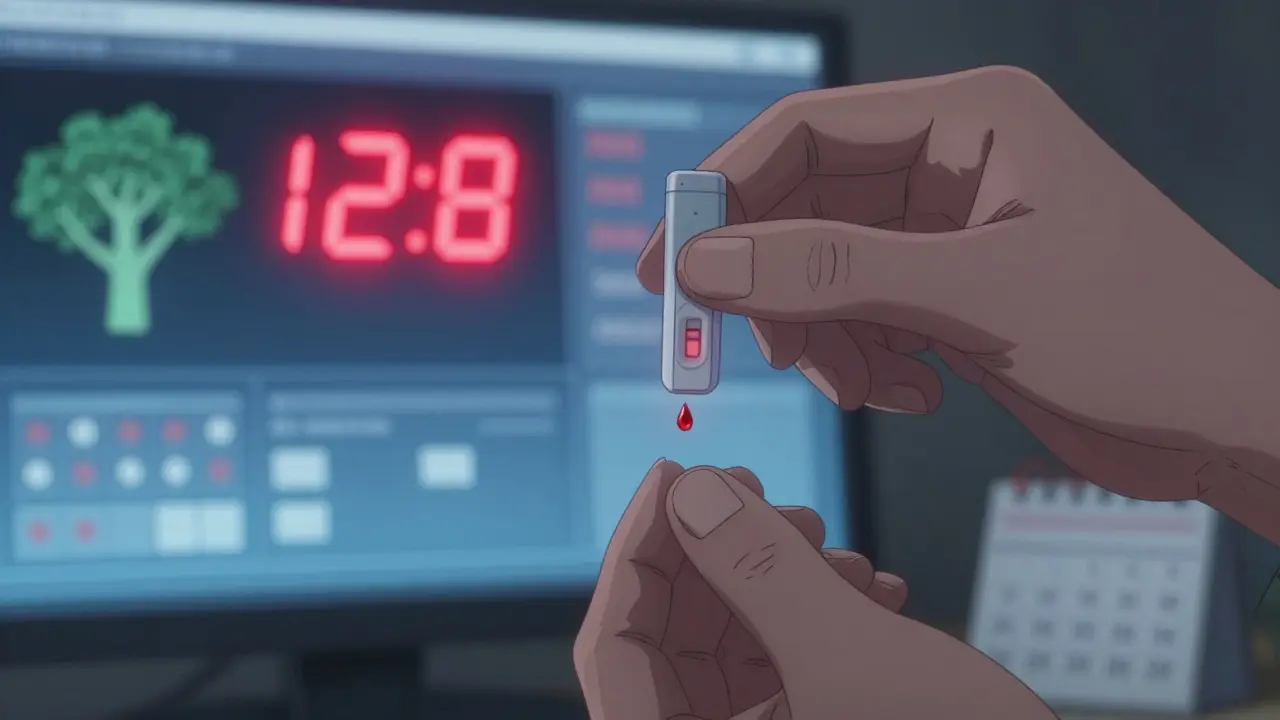
Home Testing: Is It Worth It?
Home INR monitors like the Abbott Acelis or Roche CoaguChek let you test yourself with a single drop of blood from your finger. Results come in under a minute. No waiting for the lab. No scheduling appointments. For many, it’s a game-changer.
People who test at home spend 72% of their time in the target range. Those who go to clinics? Only 58%. That’s a 14% gap-and it translates to 34% fewer clots and 21% fewer bleeds.
But it’s not for everyone. If you have shaky hands, poor eyesight, or trouble remembering to test, it’s not the right fit. The FDA reports that 25-30% of older patients struggle with home devices. And if you’re not trained properly, you can get inaccurate results. One user on Reddit said they miss the capillary tube one in five tries-wasting $6 test strips each time.
Cost is another factor. The device costs around $300. Each test strip is about $6. Medicare covers 100% for eligible patients. Private insurance usually covers most of it, but you might pay 20% coinsurance. Some people still get denied coverage and have to appeal. That’s a hassle no one needs.
Warfarin vs. Newer Blood Thinners
You might wonder: why not just switch to a newer drug like apixaban or rivaroxaban? Those don’t need INR monitoring at all. You take them once or twice a day, no blood tests, no fuss.
But here’s the thing: warfarin still has a place. If you have a mechanical heart valve, you can’t use those newer drugs. They don’t work well enough. Warfarin is the only option. Also, warfarin costs about $4 a month. The newer ones? $550-$650. That’s a huge difference if you’re paying out of pocket.
Still, the tide is turning. In 2010, 70% of blood thinner prescriptions were for warfarin. Today, it’s down to 30%. By 2028, most new patients will start on a DOAC (direct oral anticoagulant). But for the 200,000 Americans-and thousands more globally-with mechanical valves, warfarin isn’t going anywhere.
What Can You Do to Stay in Range?
Keeping your INR stable isn’t just about taking your pill. It’s about your diet, your other meds, and your routine.
- Food matters. Vitamin K makes your blood clot. Warfarin blocks vitamin K. So if you suddenly eat a lot of kale, spinach, or broccoli, your INR will drop. If you eat less, it’ll rise. Keep your intake consistent-not extreme.
- Medications interact. Antibiotics, painkillers, even some herbal supplements like garlic or ginkgo can change how warfarin works. Always tell your doctor what else you’re taking.
- Test at the same time. Test in the morning, after fasting for 4-6 hours. This reduces daily variation.
- Track your results. Use a notebook or app. Look for trends. If your INR keeps creeping up, maybe you’ve started a new supplement. If it’s dropping, maybe you’re eating more greens.
And don’t ignore the small stuff. If you’re traveling, bring extra test strips. If you’re sick, your INR can swing. Call your doctor before you change your dose-even if you feel fine.
What Happens If You Miss a Test?
Missing one test isn’t a disaster. But if you miss two in a row, you’re flying blind. Your INR could be 1.8-too low-or 5.5-too high. And you won’t know until you test.
If you miss a test and feel dizzy, have a headache, or notice unusual bruising or blood in your urine or stool, don’t wait. Go to the ER. Don’t assume it’s nothing. Bleeding can be silent until it’s not.
For those on home testing, the biggest risk isn’t the device-it’s skipping tests because you’re tired, busy, or scared of the result. But the cost of skipping? It’s not just a missed appointment. It’s your life.
What’s Next for INR Monitoring?
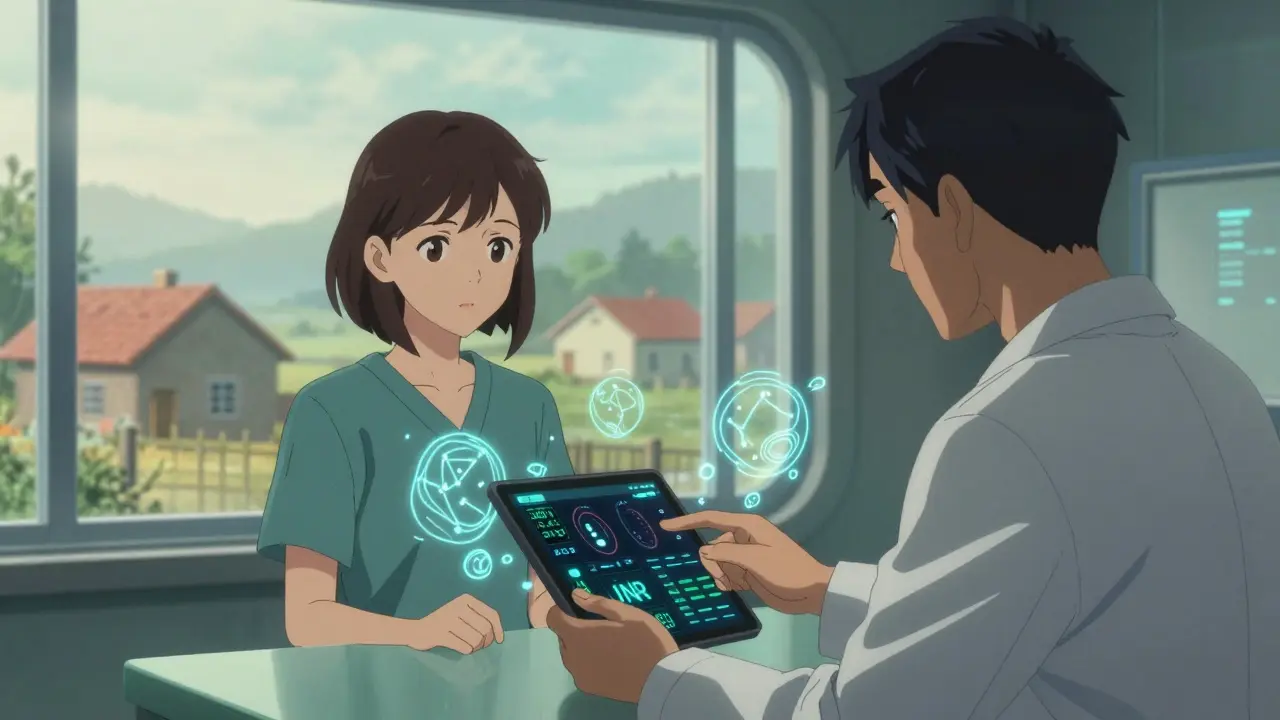
The future is connected. In early 2023, the FDA approved the first smartphone-linked INR monitor. It sends your result directly to your doctor’s system. No phone calls. No faxes. Just automatic updates.
Some clinics are even using AI to predict your next warfarin dose. One system from Mayo Clinic predicted the right dose 83% of the time. That’s better than most human adjustments.
But technology doesn’t fix everything. Rural areas still have limited access. Only 35% of rural clinics offer full anticoagulation services. That’s a problem. If you live far from a hospital, home testing might be your only option-and insurance coverage can be a nightmare.
For now, INR monitoring remains essential. It’s not glamorous. It’s not fun. But for hundreds of thousands of people, it’s the line between life and death.
What is a normal INR range for someone on warfarin?
For most people on warfarin, the target INR range is 2.0 to 3.0. This reduces the risk of blood clots without significantly increasing bleeding risk. However, people with mechanical mitral valves may need a higher range of 2.5 to 3.5. Always follow your doctor’s specific target.
How often should I test my INR?
When you first start warfarin, you may need to test every few days. Once your dose is stable and your INR stays in range for several months, monthly testing is usually enough. Some patients on home monitors test weekly, but unnecessary weekly testing is common and not always needed.
Can I check my INR at home?
Yes, home INR monitors like the Abbott Acelis and Roche CoaguChek are FDA-approved and widely used. They require a small finger-prick blood sample and give results in under a minute. They’re ideal for stable patients who are comfortable with the technique. But they’re not suitable for everyone-especially those with poor vision, tremors, or cognitive issues.
What should I do if my INR is too high?
If your INR is above 5.0, skip your next warfarin dose and contact your doctor immediately. INR levels above 4.9 significantly increase the risk of serious bleeding. Do not try to adjust your dose yourself. Your doctor may recommend vitamin K or other treatments to bring your INR down safely.
Why does my INR keep changing even if I take the same dose?
Many factors affect INR: diet (especially vitamin K-rich foods like leafy greens), alcohol, illness, new medications, and even changes in your routine. Warfarin has a narrow therapeutic window, so even small changes can shift your result. Consistency in diet and timing of tests helps stabilize your levels.
Are newer blood thinners better than warfarin?
Newer blood thinners (DOACs) like apixaban and rivaroxaban don’t require regular INR testing and have fewer food and drug interactions. They’re preferred for most patients, especially those without mechanical heart valves. But warfarin is still the only option for mechanical valve patients and is much cheaper-about $4 a month versus $550+ for DOACs.
Final Thoughts
INR monitoring isn’t a chore. It’s your safety net. It’s the quiet, daily check that keeps you alive. You don’t need to be perfect. But you do need to be consistent. Test when you’re supposed to. Track your results. Talk to your doctor when something changes. And never ignore a number that’s too high or too low.
Warfarin isn’t glamorous. But for the people who need it, it’s still the best tool we have. And with home testing, better tech, and smarter guidelines, managing your INR is easier than ever-if you stay engaged.