What to Do Right Now If Your Medication Is Recalled
It’s not rare. In 2022 alone, nearly 5,000 medications were pulled from shelves in the U.S. because of safety concerns. Most of these recalls aren’t emergencies-but if you’re taking one of the affected drugs, waiting too long to act can be dangerous. The key isn’t panic. It’s action.
Let’s say you open your medicine cabinet and see a bottle of valsartan, a blood pressure pill. You hear a recall notice on the news. Your first thought? Stop taking it. That’s the worst thing you can do.
Stopping your medication cold turkey can cause your blood pressure to spike, trigger a heart attack, or send your blood sugar into chaos if you’re diabetic. The FDA has been clear since the 2018 valsartan recall: Keep taking your medicine until your doctor or pharmacist tells you otherwise.
Check Your Lot Number-Not Just the Name
Not every bottle of a recalled drug is unsafe. Recalls target specific batches, not entire brands. A lot number is a unique code printed on the bottle, usually near the expiration date. It looks something like: A23B456 or 78901C.
According to FDA data, 45% of patients assume all versions of a drug are recalled. That’s wrong. Only 15% of recalls are Class I-the highest risk. Most are Class II or III, meaning the issue might be a mislabeled pill, a tiny bit of foreign material, or an incorrect expiration date. None of these are likely to hurt you immediately.
So what do you do? Grab your bottle. Find the lot number. Go to the FDA’s website and search for the recall notice. Type in the brand name, then filter by “Product Type: Drug.” Click on the recall alert. Match your lot number exactly. If it’s listed? You’ve got a problem. If not? You’re safe.
Call Your Pharmacy First-Don’t Wait for the Mail
Pharmacies get recall alerts before patients do. They track lot numbers, manage inventory, and know which batches are affected. If you call your pharmacy and say, “I’m on metformin, lot number B2024,” they can check their system in seconds and tell you whether your pills are safe.
The American Pharmacists Association says 92% of pharmacies have a formal recall response system. That means they can give you a replacement from a clean batch within 24 to 48 hours. Some even deliver it free. You don’t need to wait for a letter. You don’t need to schedule a doctor’s appointment right away.
And if your pharmacy says, “We don’t have your lot,” don’t assume you’re safe. Ask them to double-check. Mistakes happen. Better to be sure.
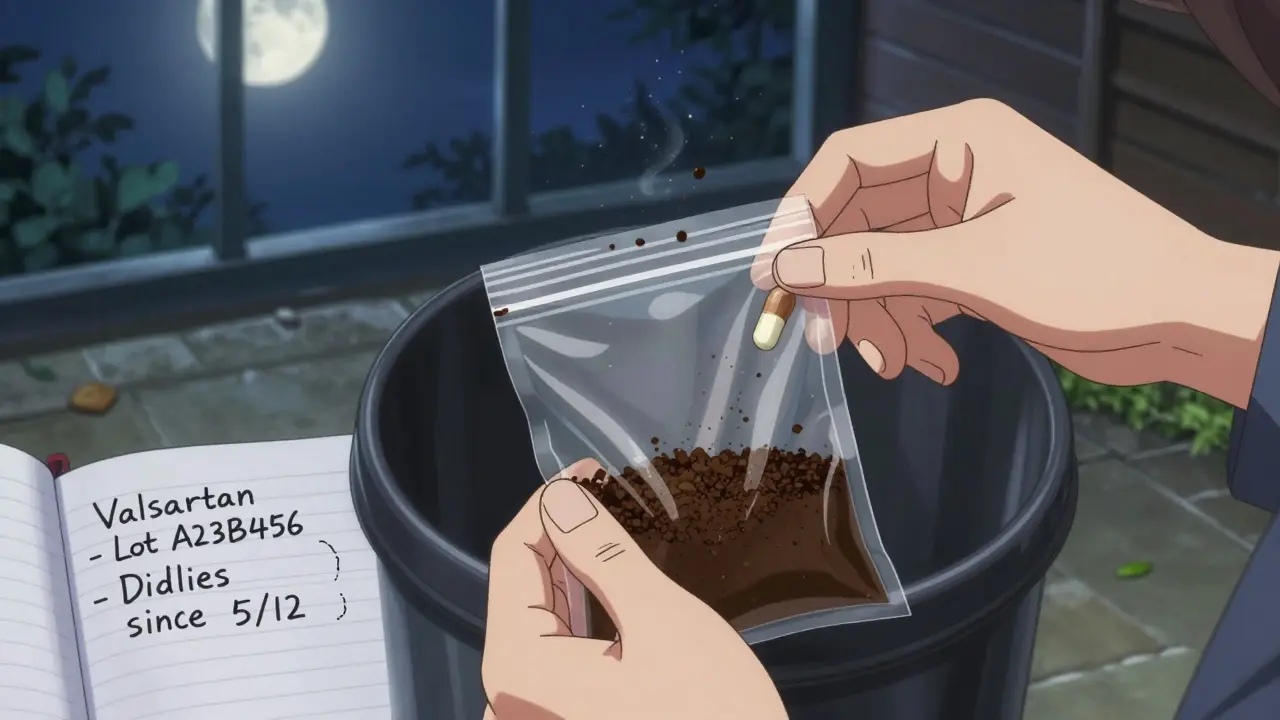
Don’t Flush, Don’t Trash-Dispose Properly
If your pharmacist confirms your medication is recalled and you’re told to stop taking it, disposal matters. Flushing pills down the toilet? That’s a no. Throwing them in the regular trash? Also a no.
The FDA recommends mixing the pills with something gross-used coffee grounds, cat litter, or even dirt. Put them in a sealed plastic bag, then toss it in the outside trash. This stops kids, pets, or even scavengers from getting into them.
Some pharmacies offer take-back bins. Call and ask. If they don’t have one, your local police station or fire department might. In Australia, many pharmacies participate in the National Drug Take-Back Program. You can drop off unused or recalled meds safely.
Watch Your Body-Even If You Think You’re Fine
Some recalled drugs don’t cause immediate harm. But they might increase your risk of long-term problems. For example, some blood pressure meds recalled in 2022 contained trace amounts of a carcinogen that builds up over time.
That’s why you need to pay attention to your body. Did you start feeling dizzy? Nauseous? Unusually tired? Have new chest pain or a rash? Write it down. Note the date, time, and what you were doing.
The FDA’s Adverse Event Reporting System got over 1.2 million reports in 2022. About 8% of those involved recalled drugs. Many patients didn’t connect their symptoms to their meds until it was too late. Keep a simple log: pill name, dose, lot number, and any changes in how you feel.
If something feels off, call your doctor. Don’t wait. Even if you think it’s “just a headache.”
Stop These 3 Common Mistakes
Most people mess up in three ways during a recall:
- Stopping medication without asking-This causes more hospital visits than the recalled drug ever did. In the FDA’s 2022 survey, 22% of patients quit cold turkey. That’s dangerous.
- Not checking lot numbers-You might be holding a safe bottle. But if you assume all are bad, you risk going without treatment.
- Improper disposal-Flushing meds pollutes water. Throwing them in the trash invites accidents. Both are preventable.
Fix these, and you’re ahead of 70% of patients.
Be Ready for Next Time
Recalls are increasing. From 2021 to 2022, they jumped 12%. Blood pressure meds, diabetes drugs, and cancer treatments are the most common. The FDA is rolling out faster digital alerts through pharmacy systems, but you can’t wait for them.
Start keeping a simple log: write down every prescription you take, including the lot number and expiration date. Do it now. Use a notebook, a note app, or a spreadsheet. Update it every time you refill.
The National Community Pharmacists Association found that patients who do this resolve recall issues 60% faster. That’s huge. You won’t be scrambling. You’ll know exactly what you have-and what to do.
Where to Find Official Recall Info
Only trust official sources. Here’s how to check:
- Go to www.fda.gov/safety/recalls
- Use the search bar-type your drug’s brand name
- Filter by “Drug” under Product Type
- Click the recall notice and compare your lot number
You can also sign up for the FDA’s free RSS feed. It sends real-time alerts to your email or phone. About 45% of healthcare pros use it. You should too.
Don’t rely on news headlines. Don’t trust Facebook posts. Don’t guess. Verify.
What Happens After a Recall?
Once a recall is issued, manufacturers have 10 business days to fix Class I issues-if they act fast. Hospitals and pharmacies are required to remove all affected products immediately. The FDA tracks every step.
But patients are the last line of defense. You’re the one holding the bottle. You’re the one who notices a new symptom. You’re the one who calls the pharmacy. Your action closes the gap between a system failure and a real health crisis.
Recalls aren’t about fear. They’re about control. You can’t stop a bad batch from being made. But you can stop it from hurting you.