It’s not uncommon to take magnesium for muscle cramps, sleep, or general wellness - and it’s just as common to be prescribed a bisphosphonate like Fosamax or Actonel for osteoporosis. But if you’re doing both, you might be accidentally ruining the effectiveness of your osteoporosis treatment. The problem isn’t that one is bad or the other is dangerous. It’s about timing. Get it wrong, and your bones could keep weakening - even if you’re doing everything else right.
Why Magnesium and Bisphosphonates Don’t Mix
Bisphosphonates are the most common pills used to treat osteoporosis. They work by slowing down the cells that break down bone, helping your skeleton stay strong. But here’s the catch: these pills are poorly absorbed to begin with. Under perfect conditions, only about 0.6% to 12% of the drug actually makes it into your bloodstream. Now add magnesium - whether it’s from a supplement, antacid, or even a laxative - and that absorption drops by 40% to 60%. The reason? Magnesium ions bind to the phosphonate part of the bisphosphonate molecule. This creates a hard, insoluble compound that your gut can’t absorb. Think of it like mixing salt into oil - they just don’t mix well, and nothing gets through. This isn’t theory. It’s been proven in clinical trials and confirmed by the FDA in the prescribing info for alendronate. If you take magnesium within two hours of your bisphosphonate, you’re basically flushing your medication down the drain.What Counts as a Magnesium Source?
Most people think only of magnesium pills. But magnesium is hiding in places you might not expect. Here’s what you need to watch for:- Over-the-counter magnesium supplements (200-400 mg per dose)
- Antacids like Milk of Magnesia (800 mg magnesium per 5 mL)
- Laxatives containing magnesium hydroxide or magnesium citrate
- Some bottled waters (San Pellegrino has about 51 mg per liter)
- Multivitamins with added magnesium
- Calcium supplements that include magnesium
The Two-Hour Rule - And Why It’s Not Optional
All major health organizations agree: you need at least two hours between your bisphosphonate and any magnesium source. That’s not a suggestion. It’s a medical requirement backed by clinical data. Here’s how to get it right:- Morning, on an empty stomach: Take your bisphosphonate first thing after waking up, with a full glass of water (8 oz). Don’t lie down for 30 minutes after.
- Wait 30 minutes: This is the standard wait time before eating or drinking anything else (coffee, juice, food).
- Wait another 90 minutes: That brings you to two full hours after taking the bisphosphonate.
- Then take magnesium: Only after those two hours have passed.
- Log it: Write it down. Use a simple notebook or phone reminder. This isn’t just advice - it’s how you track your own success.
What About IV Osteoporosis Drugs?
If you’re on an intravenous bisphosphonate like Reclast (zoledronic acid), you don’t need to worry about magnesium timing. These drugs go straight into your bloodstream - bypassing your gut entirely. That means no interaction with supplements or food. But if you’re on pills, the rule still applies. Some people ask: “Can I just switch to the IV version?” That’s something to talk to your doctor about. IV treatments are usually given once a year or every few months. They’re not for everyone - especially if you have kidney issues or can’t tolerate the infusion side effects. But if timing is a constant struggle, it’s a valid option.Real People, Real Mistakes
On Reddit’s r/Osteoporosis, users share stories that show how easy it is to mess this up. One person took Fosamax in the morning and a magnesium supplement at night - thinking that was enough. But they were also using Milk of Magnesia every few days for constipation. Their bone density didn’t improve. Another took magnesium with breakfast, then took Fosamax at lunch - not realizing breakfast still had magnesium in it from fortified cereal or a multivitamin. A Kaiser Permanente study found that patients who got written instructions with clear timing diagrams had an 89% adherence rate. Those who only got verbal advice? Only 43% got it right. That’s the difference between protecting your bones - and risking a fracture.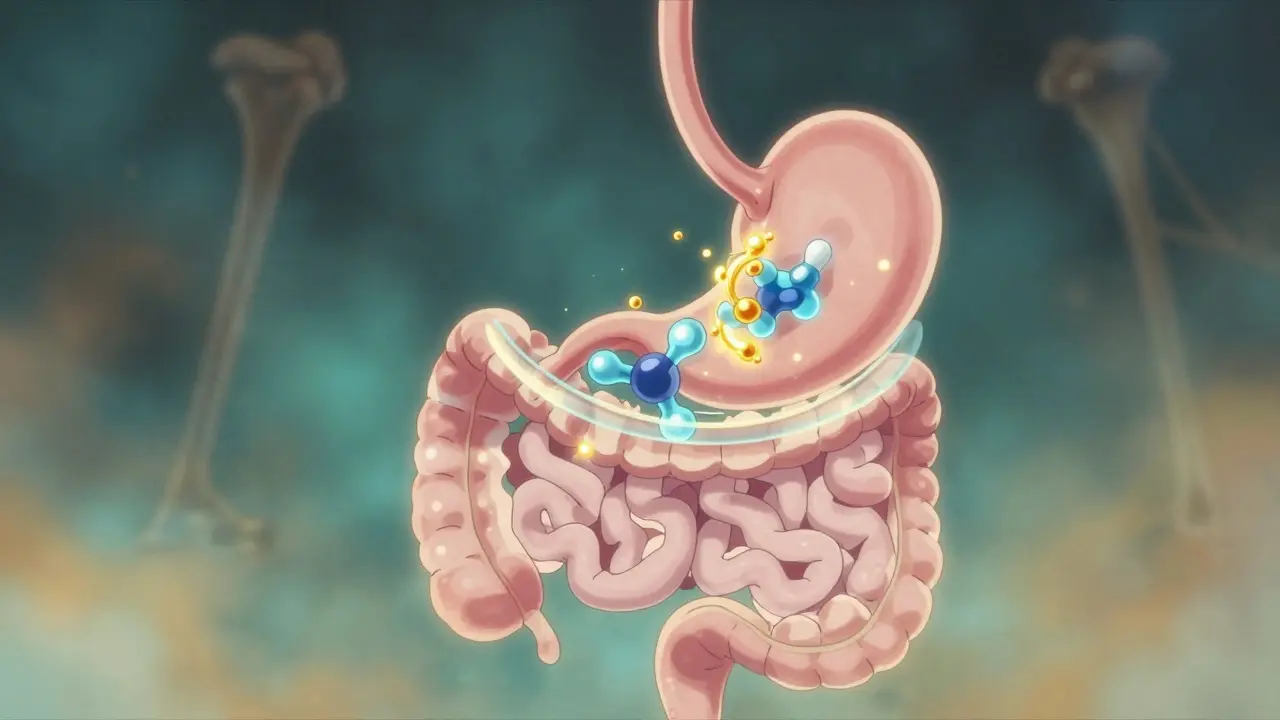
How to Stay on Track
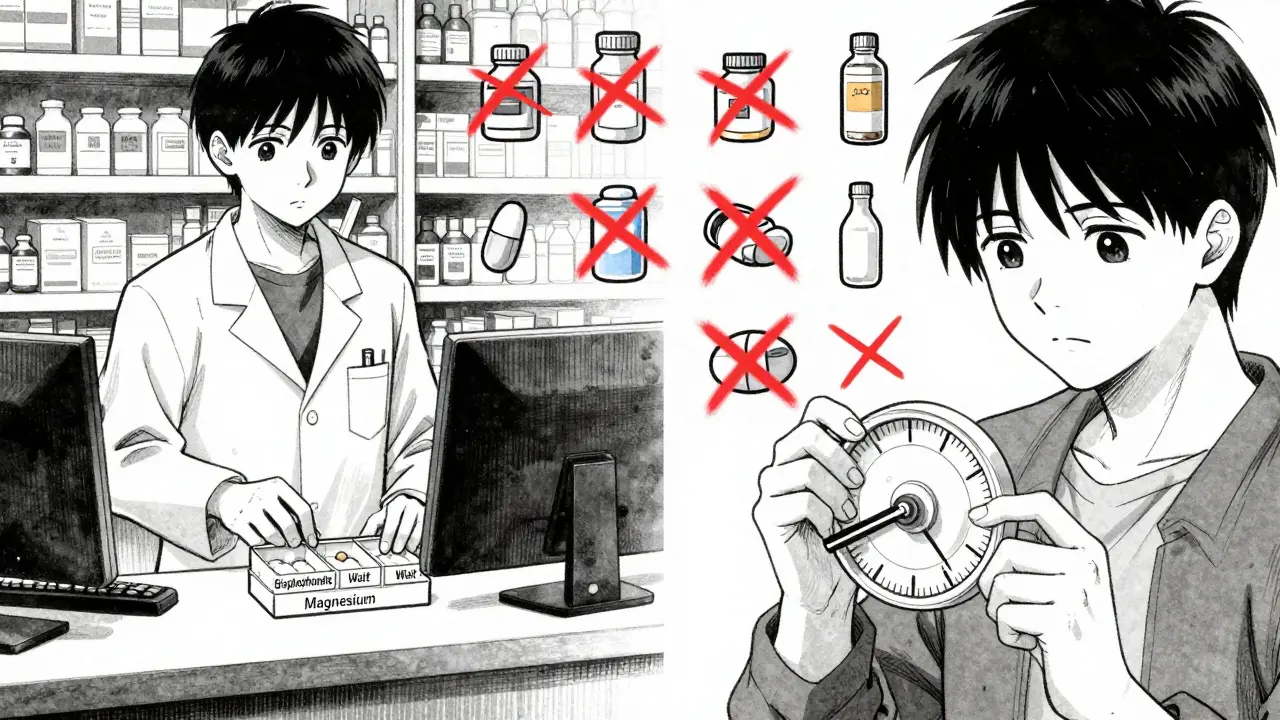
Managing multiple meds is hard. If you’re on five or more pills a day, adding a two-hour gap feels impossible. But there are tools that help:- 4-compartment pill organizers: Standard AM/PM boxes won’t cut it. You need one that separates morning, midday, afternoon, and evening doses.
- Timing wheels: These are plastic disks with hour markers. You set your bisphosphonate time, and it shows you when magnesium is safe. Clinics report a 67% success rate using these vs. 32% with paper instructions.
- Smart pill bottles: New Bluetooth-enabled bottles send reminders to your phone. A Mayo Clinic pilot study showed 92% adherence with these.
- Pharmacist counseling: Since 2023, most U.S. pharmacies are required to ask about magnesium when dispensing bisphosphonates. Don’t be shy - ask them to explain it again.
What’s Changing Soon?
The FDA now requires clear warnings on both bisphosphonate and magnesium supplement packaging - but full rollout won’t finish until 2025. Meanwhile, new formulations are in the works. Merck is testing a time-release bisphosphonate (ALN-103) that’s less affected by minerals. Early results look promising. Electronic health records like Epic and Cerner now flag this interaction automatically. If your doctor prescribes both, the system will pop up a warning. That’s good - but it doesn’t replace your own awareness. You’re still the one taking the pills.Bottom Line: Timing Saves Bones
You’re not being lazy. You’re not failing. You just didn’t know. This interaction isn’t talked about enough. But now you do. The fix is simple: take your bisphosphonate first, wait two hours, then take magnesium. That’s it. If you’ve been taking them together for months or years, don’t panic. Talk to your doctor. A bone density scan can tell you if your treatment has been working. If not, adjusting your timing could be the missing piece. Your bones don’t care about convenience. They care about consistency. And with the right timing, you can protect them - without giving up magnesium or your osteoporosis meds.Can I take magnesium and bisphosphonates at the same time if I space them out by one hour?
No. One hour is not enough. Studies show that magnesium still interferes with bisphosphonate absorption if taken less than two hours apart. The two-hour window is based on how long it takes for the stomach to empty and for the bisphosphonate to move past the absorption zone. Cutting it short reduces effectiveness by up to 50%.
Is it safe to take magnesium from food while on bisphosphonates?
Yes. Magnesium from food - like spinach, almonds, black beans, or whole grains - doesn’t interfere with bisphosphonates. The problem is with concentrated doses from supplements, antacids, or laxatives. Food-based magnesium is absorbed slowly and in small amounts, so it doesn’t create the same chemical interaction. Stick to your normal diet - just avoid supplements within two hours of your medication.
What if I forget and take them together? Should I skip my dose?
Don’t skip your bisphosphonate dose. Instead, wait until the next day and restart your schedule properly. If you took magnesium within two hours of your bisphosphonate, the dose was likely wasted - but skipping the next one won’t fix it. Just reset: take your bisphosphonate on an empty stomach tomorrow, wait two hours, then take magnesium. Consistency over time matters more than one mistake.
Do all osteoporosis medications have this interaction?
No. Only oral bisphosphonates - like alendronate (Fosamax), risedronate (Actonel), and ibandronate (Boniva) - are affected. Other osteoporosis drugs like denosumab (Prolia), teriparatide (Forteo), or raloxifene (Evista) don’t interact with magnesium. If you’re unsure which medication you’re on, check the label or ask your pharmacist. IV bisphosphonates like Reclast also don’t interact because they bypass the gut.
Can I take calcium with my bisphosphonate if I avoid magnesium?
No. Calcium also interferes with bisphosphonate absorption the same way magnesium does. You must wait at least two hours after your bisphosphonate before taking any calcium supplement. Even antacids containing calcium (like Tums) can reduce effectiveness. Stick to water only for 30 minutes after taking your pill, then wait two full hours before eating or taking any other supplement.
How do I know if my bisphosphonate is working?
Your doctor will order a bone density scan (DXA scan) every one to two years. If your bone density is stable or improving, your treatment is working. If it’s declining, timing issues - like magnesium or calcium interference - could be the cause. Don’t wait for a fracture to find out. Ask for your scan results and ask if your medication timing could be affecting them.

