Customized medications aren’t just convenient-they’re life-saving for patients who can’t tolerate commercial drugs. Maybe it’s a child who needs a dye-free, sugar-free liquid version of a pill they can’t swallow. Or an elderly patient with kidney failure who needs a dose 1/10th of the standard tablet. Or someone allergic to gluten, lactose, or dyes in every off-the-shelf option. Compounding makes these solutions possible. But every time a pharmacist mixes a batch, there’s a risk: a decimal point misplaced, a wrong ingredient pulled from the shelf, a label that says ‘5 mg/mL’ but was meant to be ‘0.5 mg/mL.’ One mistake can send someone to the ICU. And it happens more often than you think.
Why Compounding Errors Happen
Most people assume pharmacy work is all about counting pills and scanning barcodes. But compounding? That’s chemistry, precision, and human judgment rolled into one. A 2022 study in the Journal of the American Pharmacists Association found that 3-15% of compounded medications had significant deviations from the intended strength. That’s not a small number. It’s the difference between a therapeutic dose and a toxic one. The root causes are predictable. Human error. Rushed workflows. Poor labeling. Lack of training. In one case reported to the FDA, a compounded tramadol solution was labeled with concentration per container-not per milliliter. A nurse gave the full container to an elderly patient, thinking it was a single dose. The patient ended up in the ICU with serotonin syndrome. That wasn’t a freak accident. It was a failure of communication and protocol. Another common issue? Ingredient mix-ups. Pharmacists often handle dozens of powders, liquids, and capsules in a single day. If you’re not double-checking every single ingredient-its name, lot number, potency-you’re playing Russian roulette with patient safety. One pharmacy in Ohio mixed up two similar-looking powders: hydrocortisone and prednisone. The patient developed Cushing’s syndrome. The error was caught only after a follow-up blood test.USP Standards: Your Non-Negotiable Foundation
The United States Pharmacopeia (USP) sets the gold standard for compounding safety. If you’re not following USP <795> for non-sterile preparations or <797> for sterile ones, you’re operating outside of accepted practice. These aren’t suggestions-they’re the baseline for legal and safe compounding. USP <795> requires a clean, dedicated area with ISO Class 8 air quality. That means no dust, no airborne particles, no cross-contamination. It also demands that every ingredient be verified by two people. Not one. Two. One checks the label. The other checks the bottle, the certificate of analysis, and the lot number. Then they both sign off. Simple. But it’s skipped too often. For sterile compounding, USP <797> demands even more. ISO Class 5 cleanrooms. Airflow validation. Sterility testing. Media fill tests-twice a year-for every technician. And beyond-use dates (BUDs)? They’re not guesses. They’re based on real stability testing. A compounded saline solution might last 45 days if refrigerated. A cream might last 90. But if you don’t test it, you’re just guessing-and that’s not safe.Dual Verification: The Single Most Effective Tool
The American Society of Health-System Pharmacists (ASHP) says it plainly: double-check everything. Not just the math. Not just the ingredients. Everything. Here’s how it works in practice:- Pharmacist A prepares the prescription: measures the powder, adds the base, mixes the solution.
- Pharmacist B independently recalculates the dose. Uses a different calculator. Checks the formula against the original prescription.
- Pharmacist B verifies each ingredient: name, strength, expiration, source.
- Both sign the batch record. No exceptions.
Labeling: The Last Line of Defense
You can do everything right-correct calculations, clean room, dual checks-and still mess up because the label says “5 mg” instead of “5 mg/mL.” That’s what happened in 27 overdose cases between 2018 and 2022, according to the FDA. The FDA’s 2023 draft guidance is clear: always use concentration units. No more “per container.” No more “per teaspoon.” Write it like this: “10 mg/mL”. Period. Also, include the beyond-use date. The batch number. The name of the compounder. The patient’s name. The prescriber’s name. If you’re using a handwritten label, make sure it’s legible. If you’re using a printer, check that the ink doesn’t smudge. One pharmacy lost a batch because the label got wet during transport. The patient took a double dose because they couldn’t read the strength.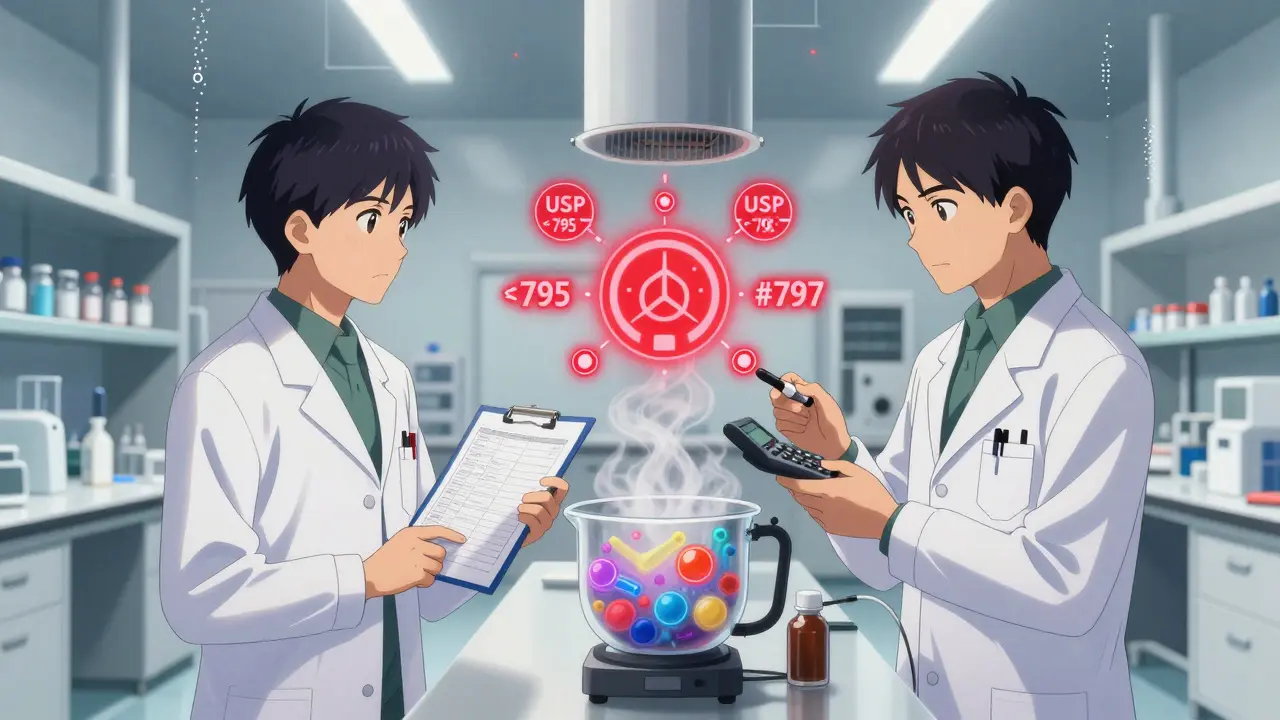
Technology That Actually Helps
Software isn’t magic. But the right software can catch mistakes before they happen. Tools like Compounding.io and PharmScript automate calculations. They flag impossible doses-like a 500 mg dose of levothyroxine for a child. They cross-check formulas against USP guidelines. They auto-generate labels with proper concentration units. One 2022 pilot study showed these systems reduced calculation errors by 40%. Even better? AI-powered tools like CompoundingGuard AI. In a 15-pharmacy trial, it cut calculation errors by 87%. It doesn’t replace the pharmacist. It just makes sure the math adds up. Barcode scanning for ingredients? That’s another game-changer. A 2021 case study at the University of Tennessee Health Science Center showed a 92% drop in ingredient misidentification after they started scanning every vial and bottle before use.Training Isn’t Optional
You wouldn’t let someone fly a plane after one lesson. Don’t let someone compound medications after a two-hour orientation. The Pharmacy Compounding Accreditation Board (PCAB) requires 40+ hours of initial training. Then 8-12 hours every year. And quarterly competency assessments. That’s not busywork. That’s how you keep skills sharp. Training should cover:- Advanced pharmaceutical math (no calculators allowed-do it by hand first, then verify)
- Aseptic technique (for sterile work)
- Chemical compatibility (what mixes, what doesn’t)
- Stability testing basics
- How to read and interpret certificates of analysis
Accreditation: The Hard Path to Trust
PCAB accreditation isn’t easy. It takes 12-18 months. Costs $15,000-$25,000. Requires 20-40 hours a month of documentation. But it works. A 2022 study in JAMA Internal Medicine found that accredited pharmacies had error rates as low as 2%. Non-accredited ones? Up to 25%. That’s not a difference in skill. That’s a difference in systems. If you’re not accredited yet, start now. It’s not just about compliance. It’s about trust. Patients and prescribers want to know you’re doing it right. Accreditation says you are.
What Happens When You Skip the Steps
The 2012 NECC outbreak killed 64 people and sickened 14,000. Why? Contaminated steroid injections. No sterility testing. No proper cleanroom. No dual verification. No oversight. That wasn’t an outlier. It was the result of years of cutting corners. Today, 35% of compounded medications are made because of drug shortages. That’s a good thing-unless the compounding pharmacy doesn’t have the infrastructure to handle it safely. The FDA says these preparations carry a 4.7 times higher risk of concentration errors. You can’t afford to be complacent. Every batch is a patient’s health on the line.Final Checklist for Error Prevention
Here’s what you need to do every single time:- Verify every ingredient with two people, using COA and physical inspection
- Recalculate every dose independently
- Use USP <795> or <797> for your environment
- Label with concentration (mg/mL), not vague terms
- Document everything: ingredients, lot numbers, equipment, environmental conditions
- Scan barcodes on all ingredients
- Test stability for BUDs-don’t guess
- Train staff quarterly, not annually
- Use compounding software with built-in safety checks
- Accredit if you can
Frequently Asked Questions
Are compounded medications FDA-approved?
No. Unlike mass-produced drugs, compounded medications don’t go through FDA clinical trials. That’s why the responsibility for safety falls entirely on the compounding pharmacy. This is why strict protocols like USP <795> and <797> are non-negotiable. If you’re compounding, you’re acting as the manufacturer-and you must meet the highest standards.
What’s the biggest cause of fatal compounding errors?
Concentration mislabeling. Errors like writing “5 mg” instead of “5 mg/mL” have led to 27 overdose incidents reported to the FDA between 2018 and 2022. A single misread label can kill. That’s why the FDA now requires all labels to use standardized concentration units. Always write it as “X mg/mL.” Never assume the prescriber or patient knows what “per container” means.
Can I use generic ingredients to save money?
Only if they’re from an FDA-registered supplier with a valid Certificate of Analysis. Generic doesn’t mean low quality-but unverified means dangerous. A 2023 FDA report found that 30% of compounding errors traced back to untested or mislabeled active ingredients. Don’t risk a patient’s life to save $50 on a powder.
How often should I test my cleanroom?
For sterile compounding (USP <797>), you need monthly air particle counts and media fill tests twice a year for every technician. For non-sterile (USP <795>), quarterly environmental monitoring is required. If you’re not testing, you’re not compliant-and you’re putting patients at risk of infection or contamination.
Is dual verification really necessary if I’m experienced?
Yes. Experience doesn’t eliminate human error-it just makes you more confident about it. A 2021 study found that even senior pharmacists made calculation mistakes 12% of the time when working under pressure. Dual verification isn’t about doubting your skills. It’s about building a safety net so no one gets hurt.

