Medication Safety Checker
How Many Medications Are You Taking?
This tool identifies potential medication risks that might go unnoticed when you're seeing only one provider
When Medications Go Wrong, It’s Not Just One Person’s Job to Fix It
Imagine taking five different pills for high blood pressure, diabetes, and arthritis. One causes dizziness. Another makes you nauseous. A third interacts badly with your supplement. You’re not sure what’s causing what-and your doctor only sees you for 12 minutes every three months. This isn’t rare. It’s normal. And that’s where the system breaks down.
For decades, healthcare ran on the idea that doctors prescribe, pharmacists dispense, and specialists treat their own slice of the puzzle. But when side effects pile up, no single person has the full picture. That’s why teams-real teams, with clear roles and shared goals-are now the only way to keep patients safe.
Pharmacists Aren’t Just the People Who Hand Out Pills
Most people think pharmacists fill prescriptions. That’s true. But in modern care, they’re the medication detectives. They know every drug interaction, every hidden side effect, every dose that’s too high or too low. In hospitals, they sit in on rounds with doctors and nurses. In clinics, they review every patient’s full list of meds-often spotting problems doctors miss.
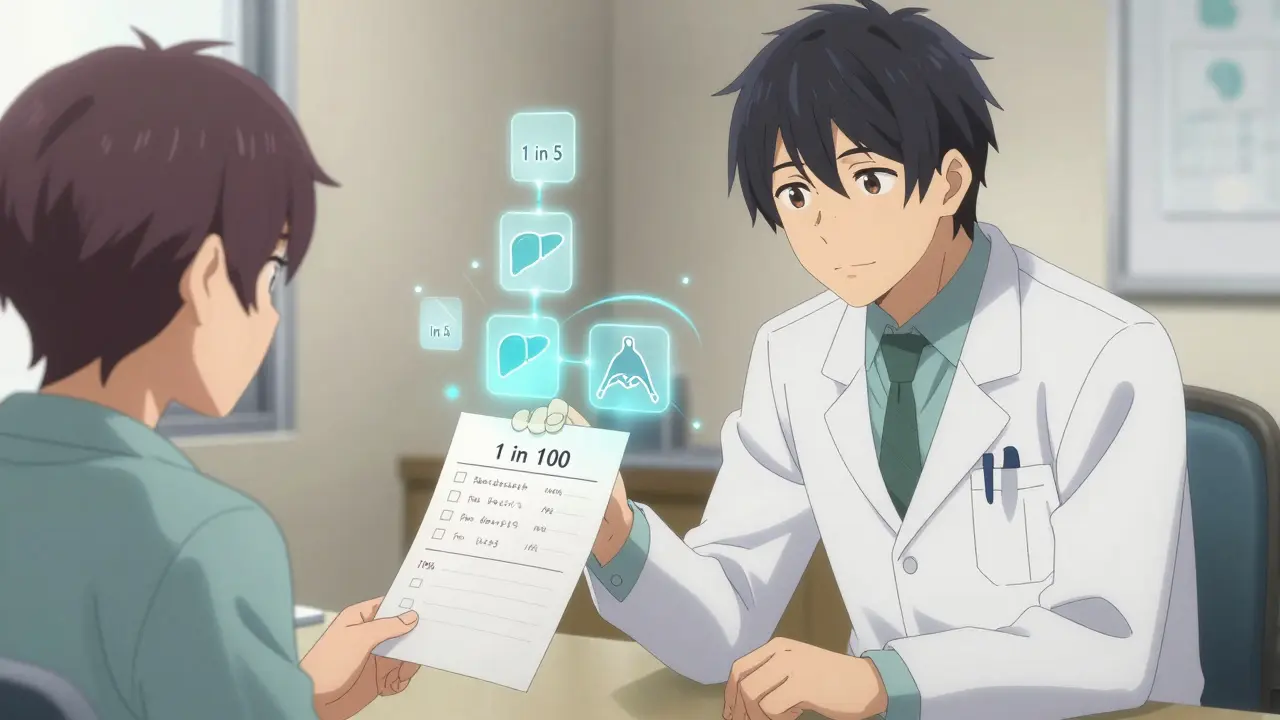
One 2022 study in JAMA Internal Medicine found that when pharmacists did full medication reconciliations, errors dropped by 67%. That means people weren’t getting the wrong pills, wrong doses, or dangerous combos. In one case, a 72-year-old man was on warfarin, ibuprofen, and an antibiotic. The pharmacist caught it: the antibiotic made the blood thinner way too strong. A simple switch prevented a hospital trip.
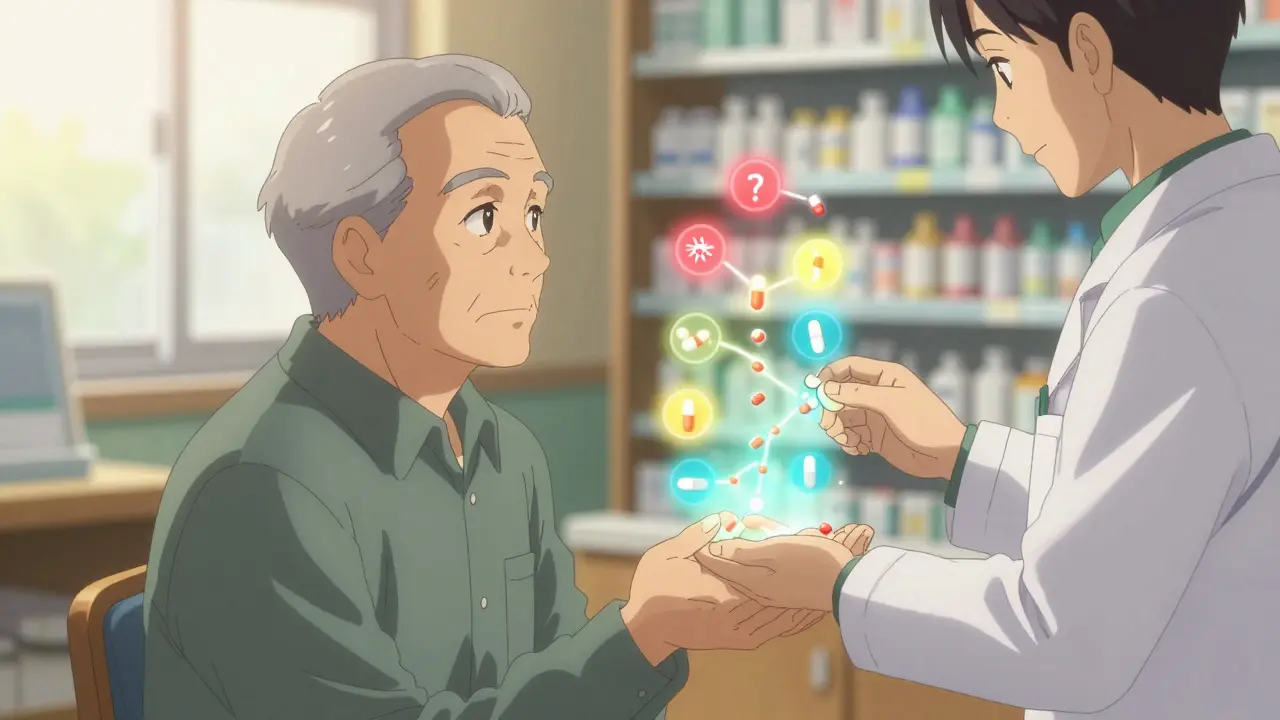
Pharmacists also know what patients aren’t saying. Someone might skip doses because the pills cost too much. Or they take them with grapefruit juice because they don’t know it’s dangerous. Pharmacists ask those questions. And they’re the ones who actually have time to listen.
Doctors Still Lead-But They Don’t Have to Do It Alone
Doctors aren’t being replaced. They’re being supported. In team-based care, doctors set the overall treatment plan-what condition needs to be treated, what goals matter most. But they rely on pharmacists to fine-tune the meds. A cardiologist might say, “We need to lower his blood pressure.” The pharmacist says, “He’s on three drugs already. One’s causing cough. Let’s swap it for a different class. And he’s not taking his diuretic because it makes him pee all night. Can we shift the dose to morning?”
This isn’t theory. In a landmark 2019 study in the New England Journal of Medicine, African-American men with uncontrolled hypertension saw their blood pressure drop to normal in 94% of cases when a pharmacist worked directly with their doctor. In the usual care group? Just 29%.
Doctors who’ve tried this say it’s not about losing control. It’s about gaining precision. A 2021 survey from the American Society of Health-System Pharmacists found that 87% of U.S. hospitals now have formal agreements letting pharmacists adjust doses, order labs, and even prescribe certain meds under agreed-upon rules. That’s not a threat. That’s a safety net.
Specialists Bring the Deep Dive-But Only When It Matters
Specialists-endocrinologists, neurologists, oncologists-are experts in their fields. But they often see patients after things have gone wrong. A patient with diabetes might see an endocrinologist for insulin, but their pharmacist is the one catching the statin that’s raising their liver enzymes. Or the antidepressant that’s making their blood sugar spike.
Team collaboration means specialists don’t work in isolation. They get real-time updates. When a cancer patient starts chemo, the oncologist tells the pharmacist: “We’re using this combo. Watch for kidney toxicity and nausea.” The pharmacist checks for interactions with the patient’s existing meds, suggests anti-nausea drugs that won’t interfere, and sets up follow-up calls to see how they’re tolerating it.
In one case, a woman on multiple drugs for lupus and depression started having seizures. Her neurologist assumed it was her disease flaring. Her pharmacist checked her med list and found a new OTC sleep aid that lowered her seizure threshold. Stop the supplement. Seizures stopped. No new scans. No hospital stay.
How This Actually Works in Practice
It doesn’t happen by magic. It takes structure.
- Shared EHRs: Everyone sees the same record. Pharmacist notes, doctor orders, specialist referrals-all in one place. Systems like HL7 FHIR make this possible.
- Daily huddles: In clinics with embedded pharmacists, teams meet for 15 minutes each day. “Who’s on a new med? Who had a side effect? Who needs a refill check?”
- Collaborative practice agreements: These are legal documents that spell out exactly what the pharmacist can do. Adjust warfarin? Order labs? Prescribe an antibiotic for a UTI? All written down. No guesswork.
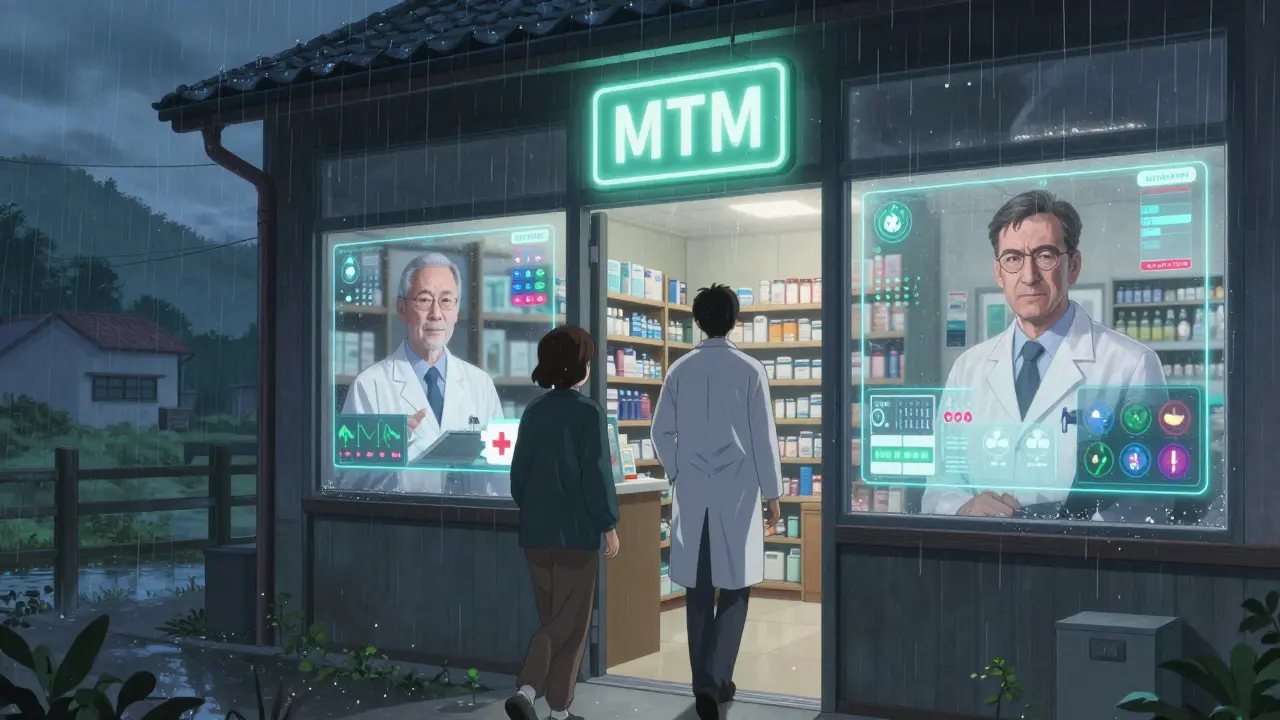
- Medication therapy management (MTM): A 30-minute session where the pharmacist walks through every pill, why it’s there, what to watch for, and how to take it right. Patients love it. 89% report higher satisfaction.
At CVS and Walgreens, over 1,200 clinics now have pharmacists working side-by-side with primary care doctors. Patients walk in, see the doctor, then sit down with the pharmacist right after. No extra appointment. No extra cost. Just better care.
The Real Impact: Fewer Trips to the ER, Fewer Side Effects
This isn’t just about feeling better. It’s about staying out of the hospital.
A 2021 review in the Journal of Interprofessional Care found that teams like this cut hospital readmissions by 23.1% and emergency visits by 15.7%. Why? Because side effects get caught early. Doses get adjusted before they cause harm. Patients understand their meds.
One community pharmacy in Ohio tracked 300 high-risk patients on five or more meds. After six months of pharmacist-led reviews, ER visits dropped by 27%. Hospitalizations fell by 32%. The biggest win? Patients stopped taking pills they didn’t need anymore.
And the cost savings? A 2023 Avalere Health analysis put it at $28.7 billion a year in the U.S. alone-just from preventing bad drug reactions and avoidable hospital stays.
Why This Still Isn’t Everywhere
It’s not perfect. And it’s not universal.
Only 28 states reimburse Medicaid for pharmacist services as of early 2024. Many doctors still don’t know how to work with pharmacists. Some see it as a threat. Others just don’t know how to start.
One physician on Sermo wrote: “It took us 8 months to get our workflow right. We had to change how we chart. How we talk. How we trust.”
Pharmacists face their own hurdles. “We cut readmissions,” says one pharmacist on Reddit, “but we spend 2.5 hours a day just filling out paperwork.”
And in rural areas? Access is still a problem. Not every town has a pharmacist who can sit in on rounds.
What’s Next? More Integration, More Power, More Patients Helped
The future is already here-just unevenly distributed.
CMS is moving toward reimbursing pharmacists directly for comprehensive medication reviews in 2025. That could open access for 28 million Medicare patients. Academic medical centers are planning to expand pharmacist roles by 92% by 2026. And by 2030, the Institute for Healthcare Improvement predicts 75% of U.S. primary care will rely on these teams.
It’s not about replacing doctors. It’s about making sure no one falls through the cracks. When a patient’s side effect isn’t just a footnote in a chart-but a shared problem the whole team solves-it changes everything.
Medications are powerful. But they’re also dangerous if used alone. The best care doesn’t come from one expert. It comes from a team that talks, listens, and acts together.
Can pharmacists really adjust my medications without my doctor’s approval?
Yes-but only if there’s a formal collaborative practice agreement in place. These are legal documents signed by both the pharmacist and the doctor that spell out exactly what changes the pharmacist can make. This could include adjusting doses, switching drugs, or ordering lab tests. It’s not random. It’s structured, documented, and always in the patient’s best interest.
Why don’t all doctors work with pharmacists?
Some are used to working alone. Others worry about losing control or don’t know how to integrate pharmacists into their workflow. There’s also a lack of reimbursement in many areas, so clinics can’t afford to hire them. But when teams do work together, 87% of hospitals report improved outcomes-and most doctors who’ve tried it say they wouldn’t go back.
Do I need to ask for this kind of care, or will my doctor offer it?
You often need to ask. In most clinics, team-based care is still the exception, not the rule. If you’re on five or more medications, have had side effects, or keep ending up in the ER, say: “Can I meet with your pharmacist for a full med review?” Many practices now offer this as a standard service, but you’ll have to bring it up.
What if my pharmacist and doctor disagree on my meds?
That’s rare, but it can happen. In well-run teams, disagreements are handled in real time-during huddles or through shared notes. If there’s a conflict, the pharmacist will usually document their concern, and the doctor reviews it. The patient is always included in the final decision. No one makes changes behind closed doors.
Is this only for people with chronic illnesses?
No. While it’s most common for people with multiple chronic conditions, anyone on multiple medications can benefit. Even if you’re on just two or three pills, a pharmacist can help you avoid interactions, reduce side effects, and save money by switching to generics. It’s not just for the sick-it’s for anyone who takes medicine.