What Really Causes Constipation?
Constipation isn’t just about not going to the bathroom often. Medically, it’s defined as having fewer than three bowel movements a week, with stools that are hard, dry, and painful to pass. It’s not rare - about one in three people in clinical settings deal with it regularly. In the U.S. alone, over 2.5 million people see a doctor for constipation every year.
The problem starts in the colon. When stool moves too slowly, the colon absorbs too much water. That turns soft waste into rock-hard lumps. Normal transit time is 24 to 72 hours. If it takes longer than that, you’re likely dealing with constipation.
There are different types, and knowing which one you have matters. About 60% of chronic cases are normal transit constipation - your colon moves stool at a normal pace, but you still strain, feel incomplete, or pass hard stools. Another 20-50% have defecatory disorders, where the muscles in your pelvic floor don’t relax properly when you try to go. Then there’s slow transit constipation, where stool crawls through the colon, taking more than 72 hours. And for 15-20% of people, symptoms stick around even after trying multiple laxatives - that’s called refractory constipation.
It’s not just about diet. Medications play a big role. Opioids cause constipation in 40-95% of users. Calcium channel blockers like verapamil and tricyclic antidepressants affect 10-30% of people taking them. Medical conditions like diabetes (affecting nearly 60% of patients), hypothyroidism, Parkinson’s disease, and spinal cord injuries are major contributors. Women are more likely to experience it, especially as they age. After 60, the risk goes up by about 1.5% every year.
How Laxatives Actually Work - And Which Ones Help
Laxatives aren’t all the same. They work in different ways, and picking the wrong one can make things worse.
Bulk-forming laxatives like psyllium or methylcellulose absorb water and swell up, making stool bigger and softer. They’re great for normal transit constipation, helping 50-60% of people. But here’s the catch: you need to drink at least 8 ounces of water with each dose. Without enough fluid, they can actually block your intestines.
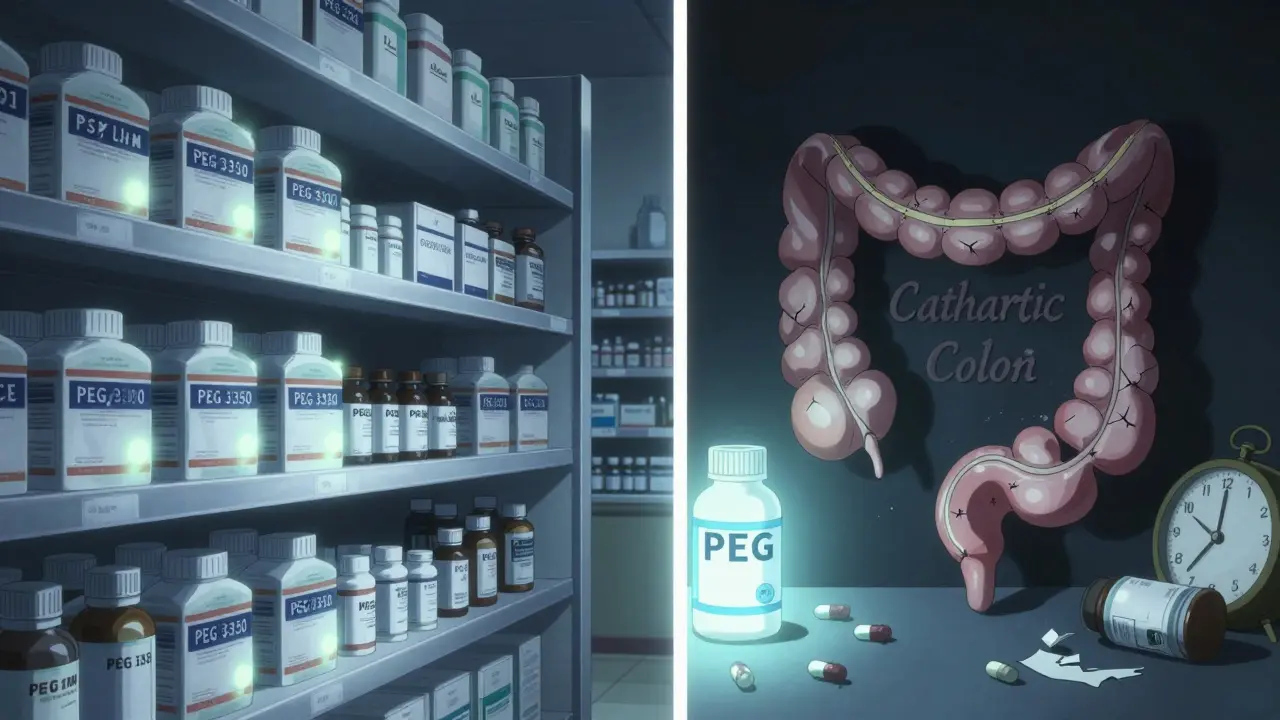
Osmotic laxatives pull water into the colon. Polyethylene glycol (PEG 3350) is the first-line choice. Studies show it works for 65-75% of people with minimal side effects. A typical dose is 17 grams a day. Lactulose and magnesium hydroxide also fall in this category. They take 1-3 days to work, so don’t expect instant relief.
Stimulant laxatives like senna and bisacodyl wake up your colon muscles. They’re fast - often working in 6-12 hours. But they’re not for long-term use. Using them for more than 12 weeks can damage your colon, leading to a condition called cathartic colon, where the muscles stop working properly. The American Gastroenterological Association says to avoid them beyond three months.
Stool softeners like docusate sodium? Don’t bother using them alone. Studies show they’re only 10-15% better than a placebo. They’re often prescribed out of habit, not science.
For stubborn cases, doctors turn to prescription options. Lubiprostone opens channels in the gut lining to pull fluid in. Linaclotide and plecanatide do something similar. They work well for people with irritable bowel syndrome with constipation, helping 40-60% of users. But they’re expensive and can cause diarrhea.
Why Fiber Alone Won’t Fix It - And What to Do Instead
Everyone says eat more fiber. But most people don’t realize how to do it right. The recommended daily amount is 25-30 grams. The average American eats only 15 grams. So yes, fiber helps - but only if you do it slowly.
Jumping from 15 to 30 grams overnight? You’ll bloat, gas, and feel worse. About 30-40% of people get bloating if they increase fiber too fast. The trick is to add 5 grams every 3-4 days. Start with oats, beans, apples, pears, and chia seeds. Soluble fiber is gentler than insoluble (like bran), so focus there.
And don’t forget water. For every 5 extra grams of fiber, drink an extra 250-500 mL of water. If you don’t, the fiber soaks up the water in your gut and makes stool harder. That’s why so many people think fiber doesn’t work - they’re not drinking enough.
Some people swear by prunes or prune juice. They’re not magic - they contain sorbitol, a natural osmotic agent. But they’re not a substitute for consistent fiber and hydration.
Behavioral Fixes That Actually Work
Medication isn’t the only answer. How you sit on the toilet matters more than you think.
Most toilets force you to sit at a 90-degree angle. That kinks your rectum and makes it harder to push. The fix? Put your feet on a small stool. This puts your hips at a 35-degree angle - like squatting. Studies show this reduces straining by 60%.
Timing matters too. The gastrocolic reflex - your body’s natural urge to go - kicks in strongest after meals, especially breakfast. Try sitting on the toilet for 10-15 minutes after eating, even if you don’t feel the urge. Don’t scroll on your phone. Just relax. Let your body do the work.
For people with pelvic floor dysfunction, biofeedback therapy works. You sit with sensors that show you how your muscles are contracting. A therapist guides you to relax them properly. After 6-8 sessions, 70-80% of people see real improvement. It’s not cheap - $100-$150 per session - but it’s often more effective than drugs.
When to Worry - Red Flags You Can’t Ignore
Most constipation is harmless. But some signs mean you need to see a doctor right away.
The American College of Gastroenterology says to get checked if you have:
- Unintentional weight loss of 10 pounds or more
- Rectal bleeding
- Change in bowel habits lasting more than 6 weeks
- A family history of colorectal cancer
These aren’t just “maybe it’s nothing” signs. They could point to something serious - like a tumor, colon obstruction, or neurological condition.
Also, if you’ve tried fiber, water, and osmotic laxatives for 4-6 weeks with no improvement, it’s time to dig deeper. Your doctor might order a colonic transit study or anorectal manometry to see what’s really going on.
Long-Term Management: What Really Works
There’s no quick fix for chronic constipation. But there is a clear path.
Start with the basics: 25-30g of fiber, 1.5-2L of water daily, and daily toilet time after breakfast. Add a footstool. Stick with it for at least a month. Most people don’t give it long enough.
If that doesn’t work, try PEG 3350 (17g daily). If you still struggle, add a stimulant laxative like senna - but only for a few weeks. Then go back to osmotic. Don’t cycle through laxatives forever. That’s how dependency starts.
For those who still can’t get relief, prescription meds like linaclotide or lubiprostone are options. But they’re expensive. And they don’t fix the root cause - they just help the symptoms.
Some people find success with magnesium citrate (250-350mg daily). It’s cheap and works for about 65-70% of users. But too much causes diarrhea, so start low.
The real win? Combining everything. One case study followed a 52-year-old woman who started with 25g of psyllium, 2 liters of water, morning coffee (to trigger the reflex), and 10 minutes of squatting on a footstool. Within 8 weeks, she was going regularly without laxatives.
What Doesn’t Work - And What to Avoid
There’s a lot of misinformation out there.
Don’t rely on enemas or herbal cleanses. They irritate the colon and don’t solve the underlying issue.
Don’t use stimulant laxatives daily for months. You risk permanent damage to your colon muscles.
Don’t think “more laxatives = better.” More doesn’t help. Consistency does.
And don’t blame yourself. Constipation isn’t a personal failure. It’s a complex condition influenced by age, gender, meds, and health history. You’re not lazy. You’re not broken. You just need the right approach.
What’s Next for Constipation Treatment
Science is moving fast. The FDA approved tenapanor in 2022 for IBS with constipation - it blocks sodium absorption in the gut to increase fluid. Early results show 45% of users get adequate relief.
Researchers are also looking at gut bacteria. The Microbiome Constipation Project found that people with chronic constipation often have low levels of Bacteroides uniformis. Probiotics targeting this could be the next big thing.
And new tech is helping. At Augusta University, doctors are using smartphone apps to analyze how people push during bowel movements. The AI can spot pelvic floor dysfunction with 85% accuracy - no expensive machines needed.
By 2030, constipation is expected to rise 12% because of aging populations and more diabetes. That means better, smarter, and more personalized care will be more important than ever.

