When you first start taking carbidopa-levodopa for Parkinson’s disease, it can feel like a miracle. The stiffness eases. Your hands stop shaking. Walking becomes possible again. But that initial relief? It doesn’t last if you don’t understand how the medicine actually works. Too many people stop taking it when they feel worse, or take it with protein-rich meals, or skip doses because they’re tired of the side effects. And then they wonder why their symptoms are coming back worse than before.
What carbidopa-levodopa really does
Carbidopa-levodopa isn’t one drug-it’s two working together. Levodopa is the active ingredient that crosses the blood-brain barrier and turns into dopamine, the brain chemical that’s missing in Parkinson’s. But if you took levodopa alone, most of it would get used up in your gut and liver before it ever reached your brain. That’s where carbidopa comes in. It blocks the enzyme that breaks down levodopa outside the brain, so more of it gets where it’s needed.
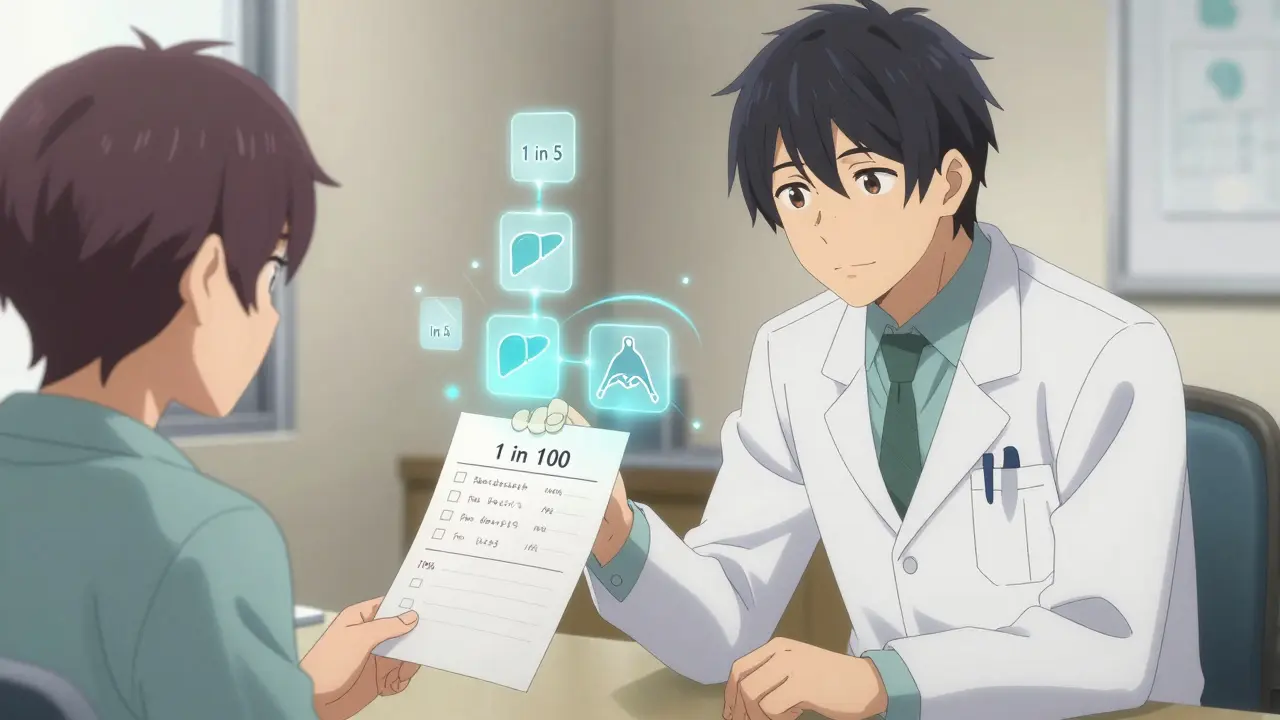
This combination is the gold standard for Parkinson’s treatment. It’s been used since the 1970s, and over 80% of people with Parkinson’s still take it today. But here’s the catch: it only works if you take it right. A 2023 study in the Journal of Neurology found that patients who received structured education about their medication had 42% fewer hospital visits for worsening symptoms over 12 months compared to those who didn’t.
Why timing matters more than you think
Levodopa competes with amino acids from food to get into the brain. That means if you take it with a steak, a cheese sandwich, or even a protein shake, it won’t work as well. The best time to take it? At least 30 minutes before eating, or an hour after. Many patients don’t know this. They take it with breakfast because that’s when they remember-and then wonder why they’re stiff again by mid-morning.
Some people try to fix this by eating low-protein meals. That’s smart-but not always easy. A dietitian who works with Parkinson’s patients in Sydney told me about a man who stopped taking his pills for weeks because he thought the nausea was from the food, not the drug. He finally figured it out after a simple conversation: "Try taking it 45 minutes before your eggs. See what happens." Within three days, his morning tremors dropped by half.
The rollercoaster of side effects
When carbidopa-levodopa first kicks in, you might feel great. Then, after a few months, you start having sudden shifts: one minute you’re moving freely, the next you’re frozen. These are called "on-off" fluctuations. They’re not a sign the medicine is failing-they’re a sign your body is adapting. Your brain’s dopamine receptors are getting sensitive. Your dosing schedule might need tweaking.
Another common side effect is dyskinesia-uncontrolled, jerky movements. It looks scary, but it’s usually a sign you’re getting enough medication. The goal isn’t to eliminate it completely-it’s to find the balance where you’re moving well most of the day, even if you have a little jitteriness for an hour or two.
People often panic when they see these movements. They cut their dose. They skip pills. They end up worse off. But if you understand that dyskinesia means the drug is working, you can work with your doctor to adjust timing or add another medication like amantadine instead of stopping what’s helping.

What most patients aren’t told
Carbidopa-levodopa doesn’t cure Parkinson’s. It doesn’t slow it down. It just replaces what your brain is losing. That means over time, you’ll need more of it, or more frequent doses. That’s normal. It’s not failure. It’s progression.
But here’s what no one tells you: the pill schedule gets more complicated as time goes on. You might start with three doses a day. Then four. Then five. Some people end up on a pump that delivers liquid levodopa directly into the intestine. That sounds extreme-but for some, it’s the only way to get stable symptom control.
Patients who get early education about this don’t feel betrayed. They feel prepared. They know the goal isn’t to avoid change-it’s to manage it.
How to get the right education
Most neurologists don’t have 45 minutes to sit down and explain every detail. That’s why you need to ask for help. Ask for a referral to a Parkinson’s nurse educator. Many hospitals have them. They’re trained to walk you through dosing, diet, side effects, and what to expect in the next year.
Don’t rely on YouTube videos or forums. Yes, they’re full of stories-but they’re also full of myths. One woman I spoke to stopped taking her pills because a forum said levodopa "burns out" dopamine cells. That’s been disproven for over 20 years. But she believed it-and her symptoms got worse.
Real education comes from trained professionals who know the science and the real-life struggles. They’ll show you how to keep a symptom diary: when you took your pill, what you ate, how you felt an hour later. That’s the key to fine-tuning your treatment.

What to do when things go wrong
Let’s say you miss a dose. Don’t double up. That can trigger severe dyskinesia or nausea. Instead, take it as soon as you remember-if it’s been less than two hours since your scheduled time. If it’s been longer, skip it and wait for your next dose. Never try to "catch up."
What if you’re vomiting and can’t keep the pill down? Try a dispersible tablet (like Sinemet CR) that you can mix with water. Or ask your doctor about a patch-there’s a new transdermal option approved in 2024 that delivers levodopa through the skin.
If you’re having freezing episodes-where your feet feel glued to the floor-try stepping over a laser line or a crack in the pavement. It sounds silly, but it tricks your brain into moving. Physical therapists who specialize in Parkinson’s teach these tricks. They’re not magic, but they work.
Real stories, real results
Maria, 68, from Melbourne, started carbidopa-levodopa in 2022. At first, she took it with her morning coffee and toast. Her tremors barely improved. She thought the medicine wasn’t working. After a visit with a Parkinson’s nurse, she learned about protein interference. She switched to taking her pills 40 minutes before breakfast, and switched her protein to lunch and dinner. Within two weeks, she was walking her dog again without stopping.
James, 72, had severe dyskinesia after three years on the drug. He was ready to quit. His neurologist added a low dose of amantadine and adjusted his dosing to every 2.5 hours instead of 3. The dyskinesia didn’t disappear-but it became manageable. He now says, "I’d rather have the shakes than be locked up."
These aren’t rare cases. They’re the norm for people who get educated early.
Bottom line: Knowledge is your best medicine
Carbidopa-levodopa is powerful. But it’s not a set-it-and-forget-it drug. It’s a tool-and like any tool, it only works if you know how to use it. The difference between someone who manages Parkinson’s well and someone who struggles isn’t always the dose. It’s the understanding.
Ask for help. Keep a diary. Talk to a Parkinson’s nurse. Learn what the side effects really mean. Don’t let fear or confusion make you stop taking something that can give you back your life.
It’s not about being perfect. It’s about being informed.
Can I take carbidopa-levodopa with food?
It’s best to take carbidopa-levodopa at least 30 minutes before eating, especially meals high in protein like meat, cheese, or beans. Protein competes with levodopa for absorption in the gut and brain, which can make the medicine less effective. If you need to take it with food to avoid nausea, choose low-protein snacks like crackers or fruit.
Why do I feel worse after taking my pill?
This is often called the "delayed on" effect. Levodopa takes 30 to 90 minutes to start working, and sometimes longer if taken with food or if your stomach is slow to empty-a common issue in Parkinson’s. If you feel worse right after taking it, it’s likely because the medication hasn’t kicked in yet, not because it’s not working. Keep a log of when you take your pill and when you feel better to spot the pattern.
Is carbidopa-levodopa addictive?
No, carbidopa-levodopa is not addictive. It doesn’t produce euphoria or cravings. But your body can become more sensitive to it over time, leading to side effects like dyskinesia or sudden "off" periods. This isn’t addiction-it’s disease progression. Never stop taking it suddenly without medical supervision, as that can cause a dangerous condition called neuroleptic malignant syndrome.
Can I stop carbidopa-levodopa if my symptoms improve?
No. Parkinson’s is a progressive condition, and carbidopa-levodopa replaces dopamine your brain no longer makes. Stopping it-even if you feel better-will cause symptoms to return quickly, often worse than before. Feeling better means the medicine is working. Don’t stop unless your doctor advises it.
What should I do if I miss a dose?
If you miss a dose and it’s been less than two hours since your scheduled time, take it as soon as you remember. If it’s been longer, skip the missed dose and wait for your next scheduled one. Never double up to make up for a missed pill-it can cause severe side effects like nausea, confusion, or uncontrolled movements.
Are there alternatives to carbidopa-levodopa?
Yes, but none are as effective for core motor symptoms. Other options include dopamine agonists (like pramipexole), MAO-B inhibitors (like rasagiline), or amantadine for dyskinesia. Some people use a levodopa infusion pump (Duodopa) or deep brain stimulation. But carbidopa-levodopa remains the most effective treatment for most people, especially in the early to mid-stages of Parkinson’s.
If you’re taking carbidopa-levodopa, you’re not just managing a disease-you’re managing a daily rhythm. The right knowledge turns confusion into control. And control means more good days.