When you’re struggling with severe obesity, diet and exercise alone often aren’t enough. That’s when many people turn to bariatric surgery. Of all the options available, two procedures dominate: gastric bypass and sleeve gastrectomy. Both help you lose weight, but they work in very different ways. And the choice between them isn’t just about which one loses more pounds-it’s about your health, lifestyle, and long-term risks.
How Each Surgery Actually Works
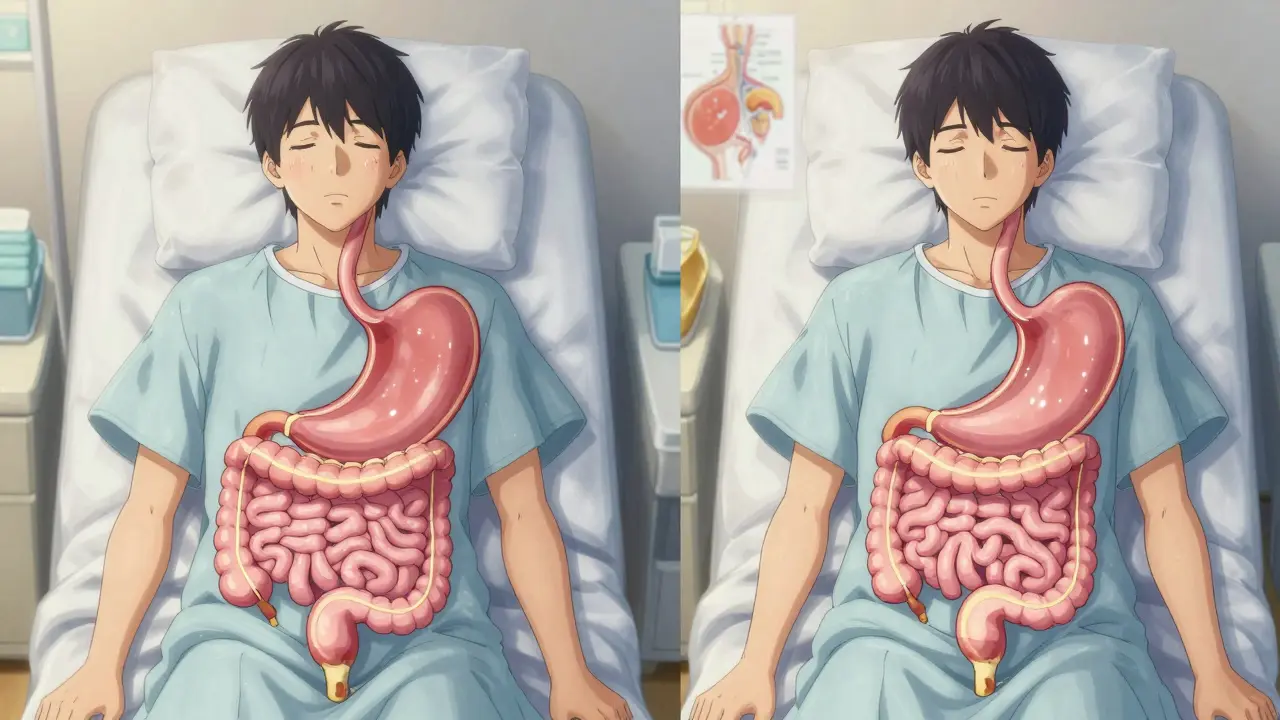
Gastric bypass, also known as Roux-en-Y gastric bypass, changes how your body digests food. Surgeons create a tiny stomach pouch-about the size of a golf ball-and connect it directly to the middle part of your small intestine. This skips most of your stomach and the first section of the intestine, so food doesn’t get fully digested. It’s not just about eating less; your body absorbs fewer calories, too. This is called a malabsorptive effect.
Sleeve gastrectomy is simpler. About 80% of your stomach is removed, leaving a long, banana-shaped tube. That’s it. No rerouting of the intestines. The new stomach holds only 2 to 5 ounces of food, so you feel full faster. But unlike gastric bypass, your digestion stays mostly normal. Food still passes through your whole digestive tract. That’s why it’s called a purely restrictive procedure.
Both are done laparoscopically-small cuts, tiny cameras, minimal scarring. Most patients leave the hospital after just one day. But the surgery time tells a story: sleeve takes about 47 minutes on average. Gastric bypass takes nearly 20 minutes longer. That extra time isn’t just busywork-it’s complexity.
Weight Loss: Who Loses More?
If your main goal is to drop the most weight, gastric bypass usually wins. Studies show that five years after surgery, gastric bypass patients lose about 57% of their excess body weight. Sleeve gastrectomy patients lose around 49%. That’s a real difference-especially when you’re talking about 80 or 100 pounds.
UPMC data confirms this trend: gastric bypass patients often lose 60-80% of excess weight within 18 months. Sleeve patients hit 60-70% over the same period, but it tends to be slower. The University of Rochester Medical Center says gastric bypass may lead to “more rapid and greater overall weight loss.”
But speed isn’t everything. Some people prefer the steady, predictable drop of the sleeve. Others hate the idea of dumping syndrome-a nasty side effect of gastric bypass where sugary or fatty foods cause sweating, nausea, and cramps. Around half to 70% of bypass patients experience it at least once. Sleeve patients rarely do.
Health Improvements: Diabetes, Blood Pressure, and More
Weight loss helps. But the real magic of bariatric surgery is how it changes your body’s hormones and metabolism. Both procedures improve type 2 diabetes, high blood pressure, sleep apnea, and cholesterol. But gastric bypass has a stronger effect on metabolic health.
Studies show that gastric bypass leads to better diabetes remission rates. Dr. Amir Ghaferi from Michigan Bariatric Surgery Collaborative says the malabsorptive part of bypass helps insulin work better. In one 2024 JAMA Network Open study, hypertension improved more often in bypass patients than in sleeve patients.
That doesn’t mean sleeve doesn’t help. Many people get off their diabetes meds after sleeve surgery. But if you have severe type 2 diabetes, gastric bypass gives you a better shot at full remission.

Risks and Complications: What Could Go Wrong?
No surgery is risk-free. But the types of risks differ.
Gastric bypass has a higher chance of serious complications in the first year: leaks, infections, blood clots, and internal hernias. But modern techniques have cut hernia risks to under 1%-thanks to closing the gaps in the intestine during surgery.
Sleeve gastrectomy is technically simpler, so it’s safer in the short term. A 2022 study of over 95,000 Medicare patients found that sleeve patients had a 32.8% lower risk of dying within five years compared to bypass patients. That’s a big deal.
But here’s the twist: sleeve patients are more likely to need a second surgery. About 3.2 percentage points more sleeve patients end up needing a revision within five years. Why? Because the stomach can stretch over time, or reflux gets worse. Some patients even develop new or worse GERD after sleeve surgery.
Gastric bypass patients don’t usually need revisions-but they face lifelong nutrient issues. Because food skips parts of the intestine, your body can’t absorb enough vitamin B12, iron, calcium, or folate. That means taking pills every day, forever. Blood tests twice a year are standard. Skip them, and you risk anemia, nerve damage, or bone loss.
Sleeve patients still need supplements, but less often. Annual blood tests are usually enough. That’s a major reason why more people choose sleeve-it’s easier to manage long-term.
Cost, Insurance, and Recovery
Cost matters. In 2024, sleeve gastrectomy averaged $14,500 out-of-pocket after insurance. Gastric bypass? Around $19,300. That’s a $4,800 difference. Most insurers cover both if your BMI is 40 or higher, or 35 with conditions like diabetes or high blood pressure. But some, like UnitedHealthcare, now require a BMI of 45.
Recovery time is similar-2 to 4 weeks off work. But diet progression is different. After gastric bypass, you have to avoid sugar, fat, and carbonated drinks for months. After sleeve, you can eat more normally, sooner. That’s why many patients say recovery feels easier with the sleeve.
What Patients Really Say
Reddit’s r/bariatrics community has over 1,200 posts comparing the two. Sleeve patients often say: “I recovered faster,” “I didn’t get dumping,” “I can eat regular food.” But many also say: “I’m hungry again after a year,” “I didn’t lose as much as I hoped.”
Gastric bypass patients say: “I lost 100 pounds in a year,” “My diabetes disappeared,” “I feel like a new person.” But they also say: “I’m on supplements every day,” “I can’t eat cake anymore,” “I had to go back to the hospital for a blockage.”
RealSelf.com, a patient review site, gives gastric bypass a 91% “Worth It” rating and sleeve a 89%. But the complication rate for bypass is 18% versus 12% for sleeve. So the higher satisfaction comes with more risk.
Why Sleeve Is Becoming the Most Popular
In 2010, sleeve gastrectomy made up less than 10% of bariatric surgeries. By 2023, it was over 63%. Gastric bypass dropped from 31% to 27%.
Why? Simplicity. Lower short-term risk. Fewer supplements. Faster recovery. Patients want less complexity. Surgeons prefer it too-it’s quicker, cheaper, and easier to teach.
But the trend doesn’t mean bypass is outdated. It still delivers better long-term weight loss and metabolic results. The choice isn’t about what’s trending-it’s about what fits your body and your life.
Who Should Choose Which?
Choose gastric bypass if:
- You have type 2 diabetes or severe metabolic disease
- You need the most weight loss possible
- You’re willing to take lifelong supplements and get regular blood tests
- You can handle dietary restrictions and avoid sugar/fat
Choose sleeve gastrectomy if:
- You want a simpler procedure with fewer complications
- You prefer less dietary restriction after surgery
- You want to avoid dumping syndrome
- You’re okay with potentially slower weight loss or needing a revision later
There’s no perfect choice. Both surgeries change your life. The best one is the one that matches your health goals, your risk tolerance, and your willingness to stick with lifelong habits.
What’s Next?
Surgeons are now experimenting with hybrid procedures-like a sleeve with a mini-bypass-to get the benefits of both. Early trials at Mayo Clinic and Massachusetts General are promising. But for now, the two main options remain the same.
If you’re considering surgery, talk to a bariatric specialist. Don’t just pick the most popular one. Look at your bloodwork, your diabetes status, your eating habits, and your long-term goals. This isn’t a one-size-fits-all decision. It’s a personal one.
And remember: surgery isn’t the end. It’s the beginning. The real work starts after the scars heal.
Which surgery leads to more weight loss: gastric bypass or sleeve gastrectomy?
Gastric bypass typically leads to more weight loss. On average, patients lose 57% of their excess body weight five years after bypass, compared to 49% after sleeve gastrectomy. Gastric bypass also tends to produce faster initial results, with many patients losing 60-80% of excess weight within 18 months. The malabsorptive component of bypass helps burn more calories, giving it an edge in long-term weight reduction.
Is sleeve gastrectomy safer than gastric bypass?
Yes, in the short term. A 2022 study of over 95,000 patients found that sleeve gastrectomy had a 32.8% lower risk of death within five years compared to gastric bypass. It also has fewer immediate complications like leaks and infections. However, sleeve patients are more likely to need a revision surgery later-about 3.2 percentage points more than bypass patients-often due to stomach stretching or worsening reflux.
Do I need to take supplements after bariatric surgery?
Yes, but the amount and frequency differ. Gastric bypass patients must take lifelong supplements for vitamin B12, iron, calcium, and folate because the surgery blocks nutrient absorption. Blood tests are recommended twice a year. Sleeve gastrectomy patients still need supplements, but less frequently-usually once a year-because digestion remains mostly intact. Skipping supplements after bypass can lead to anemia, nerve damage, or osteoporosis.
Can I eat normally after sleeve gastrectomy?
You can eat a wider variety of foods after sleeve gastrectomy compared to gastric bypass. There are fewer strict dietary rules, especially around sugar and fat. Most patients return to regular meals within a few months. However, portion sizes must still be small, and overeating can stretch the stomach over time. Gastric bypass patients must avoid sugar and fatty foods completely to prevent dumping syndrome, a painful reaction that causes nausea, sweating, and dizziness.
Why is sleeve gastrectomy more popular than gastric bypass?
Sleeve gastrectomy is more popular because it’s simpler, faster, and has fewer immediate risks. It doesn’t involve rerouting the intestines, so there’s less chance of malabsorption or internal hernias. Patients recover faster, need fewer supplements, and report less dietary restriction. In 2023, over 63% of bariatric surgeries in the U.S. were sleeves, up from less than 10% in 2010. Surgeons and patients both favor it for its lower complexity and better short-term safety profile.
Does bariatric surgery cure type 2 diabetes?
It can, especially with gastric bypass. Studies show that 60-80% of patients with type 2 diabetes go into remission after bypass surgery, often within weeks. Sleeve gastrectomy also improves or resolves diabetes in about 50-70% of cases. The difference comes from how bypass affects gut hormones and insulin sensitivity. If diabetes is your main concern, gastric bypass offers the strongest chance of long-term remission.
How much does bariatric surgery cost?
As of 2024, the average out-of-pocket cost for sleeve gastrectomy is $14,500, and for gastric bypass, it’s $19,300-after insurance covers about 80%. Costs vary by region and hospital. Most insurers require a BMI of 40 or higher, or 35 with obesity-related conditions like diabetes or high blood pressure. Some insurers, like UnitedHealthcare, now require a BMI of 45.
Can I get pregnant after bariatric surgery?
Yes, but timing matters. Doctors recommend waiting 12 to 18 months after surgery to conceive. This gives your body time to stabilize weight and nutrient levels. Pregnancy after gastric bypass requires extra monitoring because of nutrient absorption issues. Women who’ve had sleeve surgery generally have fewer complications during pregnancy, but both groups need regular blood tests and prenatal supplements.