Introduction: Understanding Autoimmune Diseases and Mouth Sores
As someone who has experienced mouth sores and has an interest in autoimmune diseases, I've always been curious about the possible connection between the two. In this article, I will be discussing the relationship between autoimmune diseases and mouth sores, as well as their common triggers and treatment options. Together, we will explore the various aspects of these conditions and how they may be interconnected.
What are Autoimmune Diseases?
Autoimmune diseases are a group of conditions in which the immune system mistakenly attacks the body's own healthy tissues. This can result in inflammation and damage to various organs and systems in the body. There are more than 80 different types of autoimmune diseases, with some of the most common ones being rheumatoid arthritis, lupus, and multiple sclerosis. These conditions can manifest in a variety of ways, with symptoms ranging from mild to severe, and can significantly impact an individual's quality of life.
What are Mouth Sores?
Mouth sores, also known as oral ulcers or canker sores, are small, painful lesions that develop inside the mouth or on the gums. They can occur as a single sore or multiple sores and can vary in size and appearance. Mouth sores are quite common and can affect people of all ages. While they are usually harmless and heal on their own within a week or two, they can be quite bothersome and uncomfortable, making it difficult to eat, drink, or speak.
The Link between Autoimmune Diseases and Mouth Sores
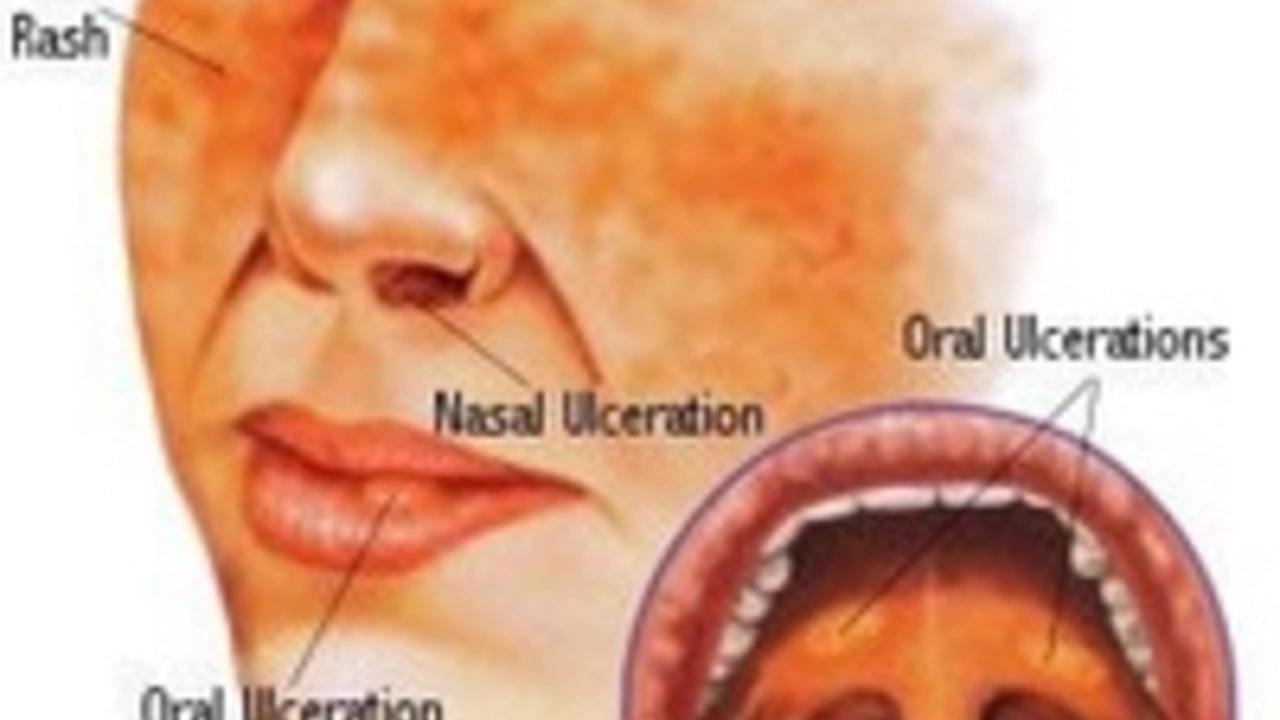
There is a growing body of evidence suggesting a connection between autoimmune diseases and mouth sores. Many autoimmune diseases can cause inflammation in various parts of the body, including the mouth. This inflammation may lead to the development of mouth sores. Some of the autoimmune diseases that have been associated with mouth sores include:
- Behcet's disease
- Lupus
- Celiac disease
- Crohn's disease
- Sjogren's syndrome
It's important to note that not everyone with an autoimmune disease will experience mouth sores, and the severity of the sores can vary greatly from person to person. However, if you have an autoimmune disease and frequently experience mouth sores, it's essential to discuss this with your healthcare provider, as it could be an indication of your disease's activity or severity.
Common Triggers for Mouth Sores in Autoimmune Diseases
Several factors can trigger the development of mouth sores in individuals with autoimmune diseases. Some of these triggers may include:
- Stress
- Hormonal changes
- Food sensitivities or allergies
- Vitamin deficiencies
- Certain medications
- Oral trauma or injury
Understanding and identifying these triggers can help in managing and preventing mouth sores. If you have an autoimmune disease and are prone to mouth sores, it may be helpful to keep track of potential triggers and discuss them with your healthcare provider to develop a personalized management plan.
Treatment Options for Mouth Sores
While mouth sores associated with autoimmune diseases can be bothersome and painful, there are several treatment options available to help alleviate symptoms and promote healing. Some of these treatments include:
- Over-the-counter pain relievers
- Topical anesthetics or anti-inflammatory creams
- Mouth rinses containing steroids or antimicrobial agents
- Oral medications to suppress the immune system
- Addressing underlying vitamin deficiencies or food sensitivities
It's important to work closely with your healthcare provider to determine the most appropriate treatment options for your specific needs and to monitor any potential side effects or complications.
Conclusion: The Importance of Awareness and Management
The connection between autoimmune diseases and mouth sores is an important one to be aware of, as it can have a significant impact on an individual's overall health and well-being. If you have an autoimmune disease and are experiencing mouth sores, it's essential to discuss this with your healthcare provider and develop a comprehensive management plan. By understanding the potential triggers and treatment options, you can work towards minimizing the frequency and severity of mouth sores and improve your overall quality of life.