Prescriber Override: When Doctors Bypass Rules for Your Safety
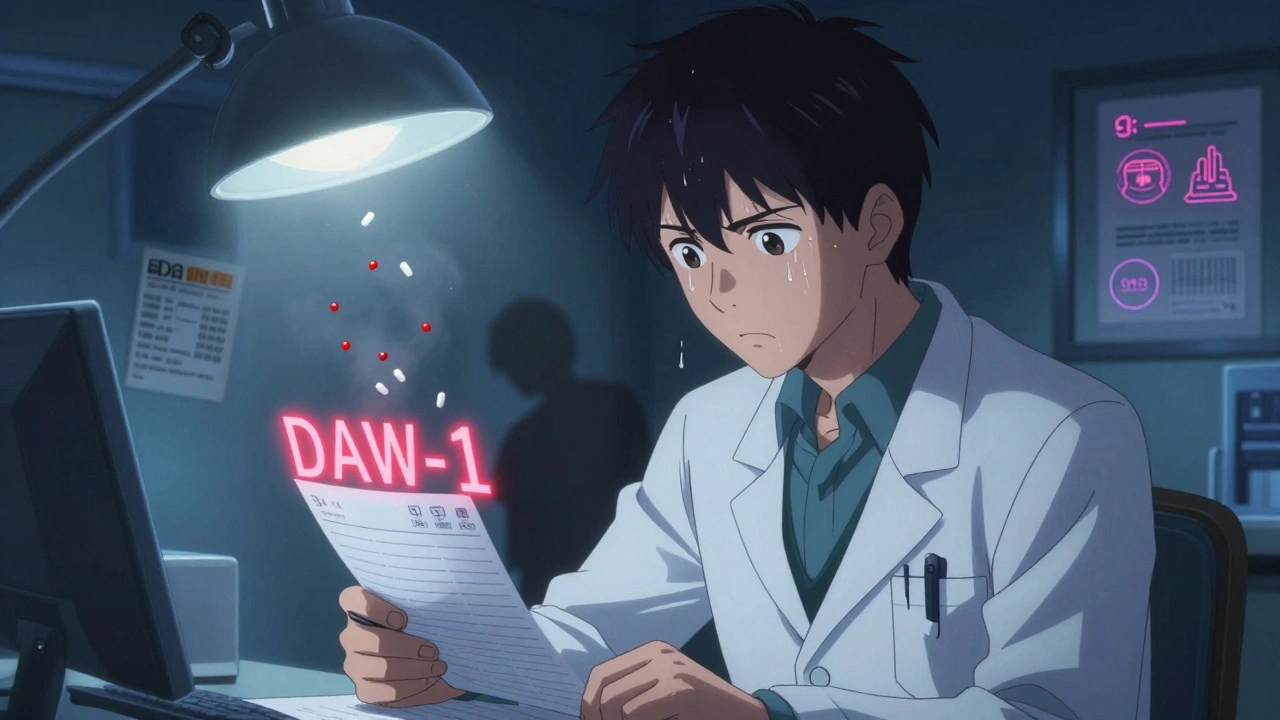
When a pharmacist refuses to fill a prescription because of a potential drug interaction or dosage issue, a prescriber override, a clinical exception that allows a provider to bypass automated safety alerts in the pharmacy system. Also known as a provider override, it’s not a loophole—it’s a safety valve. These alerts exist to prevent dangerous mistakes, but they don’t always understand your full story. Sometimes, the risk of not taking a medication is greater than the risk of a interaction. That’s when your doctor steps in.
A prescriber override, a clinical exception that allows a provider to bypass automated safety alerts in the pharmacy system. Also known as a provider override, it’s not a loophole—it’s a safety valve. These alerts exist to prevent dangerous mistakes, but they don’t always understand your full story. Sometimes, the risk of not taking a medication is greater than the risk of a interaction. That’s when your doctor steps in.
Think of it like this: your pharmacy system is programmed with rules based on population data. But you’re not a statistic. You might be on blood thinners and need an antibiotic that technically interacts—but your infection is severe, and stopping the antibiotic could be riskier. Or you’re on multiple medications for heart disease, and one of them triggers a warning, but your doctor knows you’ve taken it for years with no issues. In cases like these, the override isn’t ignoring safety—it’s applying clinical judgment.
It’s not just about drug interactions. Overdose alerts, duplicate therapy flags, and age-based restrictions can all trigger a prescriber override. A 70-year-old on a blood pressure med might get flagged for adding a new pain reliever, even if it’s the only one their kidneys can handle. A diabetic might need a higher insulin dose than the system allows, because their body has changed. These aren’t errors in the system—they’re gaps in its ability to see the person behind the chart.
But overrides aren’t automatic. Your doctor has to justify them—usually by typing a note explaining why the alert was overridden. That note becomes part of your record. It’s not a free pass. Pharmacies track these overrides closely, and regulators review them to spot patterns. Too many overrides from one provider? That raises a red flag. Too few, even when needed? That could mean patients are going without vital meds.
And here’s what matters most: you should know when one has happened. If your pharmacy says, "Your doctor had to override a safety alert," don’t just accept it. Ask why. Was it because of a drug interaction? A dosage limit? A duplicate? Then ask: "Is this still safe for me?" You have the right to understand what’s being changed and why. That’s part of your medication safety, the practice of ensuring drugs are used correctly to avoid harm. Also known as pharmaceutical safety, it’s the foundation of every prescription you take.
Some people worry overrides mean the system is broken. But it’s not broken—it’s incomplete. Automated systems catch obvious risks, but they can’t replace a doctor who knows your history, your allergies, your lifestyle, your fears. The best safety system combines both: smart alerts, and smart people who know when to ignore them.
In the posts below, you’ll find real-world examples of when overrides matter—from insulin reactions to blood thinner risks, from fiber blocking absorption to switching BPH meds. These aren’t theoretical scenarios. They’re daily decisions made by doctors, pharmacists, and patients who understand that rules exist to serve people, not the other way around.
Prescriber Override: When Doctors Can Require Brand-Name Drugs Instead of Generics
- Elliot Grove
- on Dec 8 2025
- 10 Comments