Generic Substitution: What It Is and Why It Matters for Your Health and Wallet
When your pharmacist hands you a pill with a different name than what your doctor wrote, that’s generic substitution, the practice of swapping a brand-name drug for a chemically identical generic version approved by the FDA. Also known as drug substitution, it’s one of the most common and safest ways to cut prescription costs without losing effectiveness. This isn’t a trick or a shortcut—it’s science-backed policy built into how the U.S. healthcare system works.
Behind every generic drug is a process called bioequivalence testing, a strict FDA requirement that proves the generic delivers the same amount of active ingredient into your bloodstream at the same rate as the brand-name version. If it doesn’t pass, it doesn’t get approved. That’s why pharmacists can legally swap them—and why doctors trust them. The Therapeutic Equivalence Codes, the FDA’s system for labeling which generics are interchangeable with brand drugs, tells pharmacists exactly which swaps are safe. You’ll see these codes in the FDA Orange Book, the official public database that lists all approved drug products and their therapeutic equivalence ratings. It’s not guesswork. It’s a clear, tested roadmap.
Some people worry that generics are "inferior" or "cheap copies." That’s a myth. Generics have the same active ingredients, strength, dosage form, and route of administration. The only differences? The shape, color, or inactive fillers—and the price, which is often 80% lower. You’re not getting less medicine. You’re getting the same medicine without the brand markup.
Generic substitution isn’t just about saving money—it’s about access. For people on insulin, blood pressure meds, or antidepressants, switching to a generic can mean the difference between taking their medicine every day or skipping doses because of cost. It’s not a compromise. It’s a smart, safe choice backed by decades of real-world use and clinical data.
But it’s not automatic. You still have the right to ask for the brand if you need it. You can also ask your pharmacist to explain why a substitution was made. And if you’ve had a reaction before, or if your condition is sensitive—like epilepsy or thyroid disease—you should talk to your doctor before any switch. Not all generics are created equal in every situation, even if they’re technically equivalent.
Below, you’ll find clear, no-fluff guides on how generic substitution actually works, what to watch for, how to talk to your doctor about it, and why authorized generics might be an even better option than standard generics. Whether you’re switching your blood pressure pill, your antidepressant, or your cholesterol med, these posts give you the facts you need to make confident, informed decisions—without the jargon or the hype.
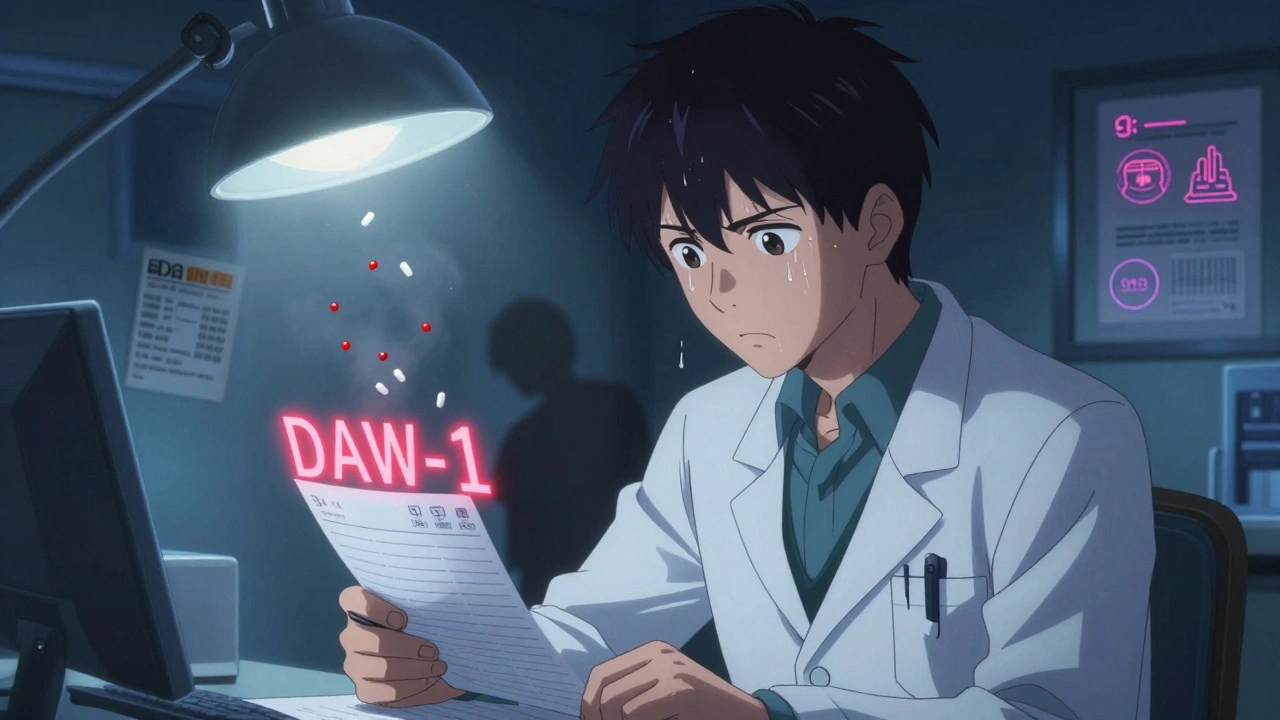
Prescriber Override: When Doctors Can Require Brand-Name Drugs Instead of Generics
- Elliot Grove
- on Dec 8 2025
- 10 Comments