Understanding the Basics of Acne
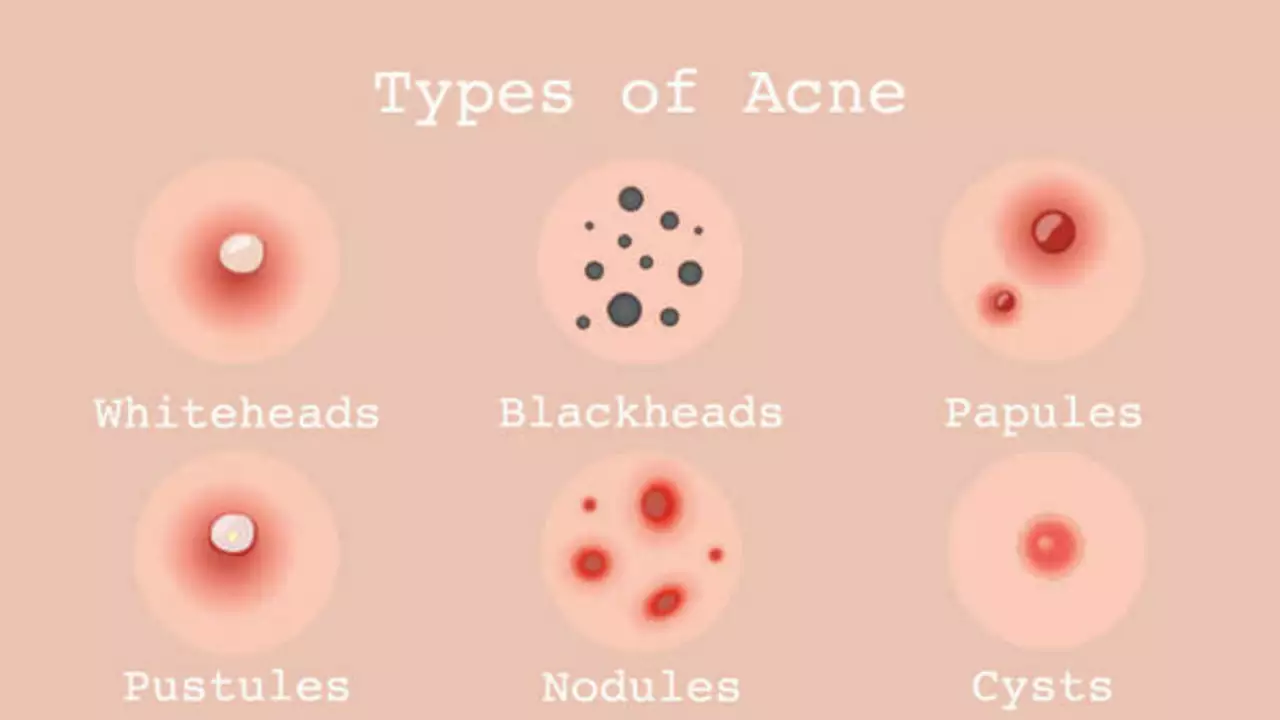
Before we delve into the details of nodular and cystic acne, it's important to understand what acne is. Acne is a skin condition that occurs when your hair follicles become clogged with oil and dead skin cells. It often causes whiteheads, blackheads or pimples, and usually appears on the face, forehead, chest, upper back and shoulders. Acne is most common among teenagers, though it affects people of all ages. There are several types of acne, including nodular and cystic acne, which we will discuss in detail.
Defining Nodular Acne
Nodular acne is a severe type of acne that causes hard, painful nodules or lumps to form under the skin. These nodules can be large and long-lasting, and they often leave behind scars. Nodular acne can affect anyone, but it is more common in teenagers and young adults. It is caused by an excess production of oil, an accumulation of dead skin cells, and the presence of acne-causing bacteria. This leads to inflammation and the formation of nodules.
Recognizing the Symptoms of Nodular Acne
It's crucial to be able to recognize the symptoms of nodular acne. These can include hard, painful lumps under the skin, red or purple discoloration, and a tendency to scar. Unlike other forms of acne, nodular acne does not typically involve many blackheads or whiteheads. It's important to seek treatment for nodular acne, as it can be painful and can lead to permanent scarring.
Defining Cystic Acne
Cystic acne, like nodular acne, is a severe form of acne. However, it differs in that it involves the formation of cysts. These cysts are soft, fluid-filled lumps beneath the skin. They can be extremely painful, and they often lead to scarring. Cystic acne is caused by the same factors as nodular acne: excess oil, dead skin cells, and acne-caicing bacteria. However, in the case of cystic acne, the pores become blocked, leading to the formation of cysts.
Recognizing the Symptoms of Cystic Acne
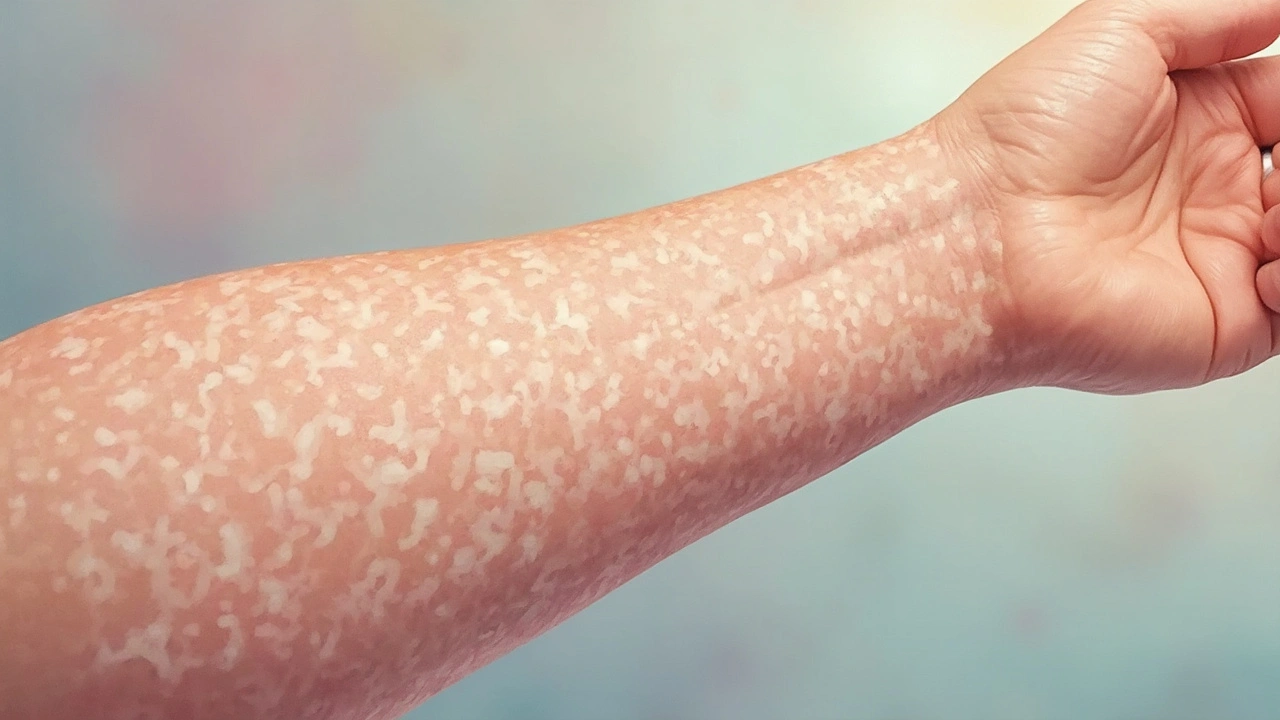
The symptoms of cystic acne include large, red, painful, pus-filled cysts, as well as areas of skin that are red and swollen. It is also common to experience scarring with cystic acne. This type of acne can also affect large areas of the skin, and it can occur on the face, chest, back, arms, and even the thighs. Because of the severity of cystic acne, it is important to seek treatment as soon as possible.
Key Differences Between Nodular and Cystic Acne
Despite their similarities, there are key differences between nodular and cystic acne. For one, the physical characteristics of the acne are different, with nodular acne causing hard, painful nodules and cystic acne causing soft, fluid-filled cysts. Additionally, cystic acne tends to be more painful and more likely to cause scarring than nodular acne. Finally, while both types of acne can occur anywhere on the body, nodular acne is more common on the face, while cystic acne often affects larger areas of the body.
Treatment Options for Nodular and Cystic Acne
Both nodular and cystic acne are serious conditions that require treatment from a dermatologist. Treatment options may include oral medications, topical treatments, or even surgical procedures. Additionally, lifestyle changes such as improving diet, reducing stress, and maintaining a consistent skincare routine can also help manage these conditions. It's important to remember that treatment can take time, and it may take several weeks or even months to see improvement.
Prevention Tips for Nodular and Cystic Acne
While it is not always possible to prevent nodular or cystic acne, there are steps you can take to reduce your risk. These include maintaining a healthy diet, avoiding pore-clogging cosmetics, keeping your skin clean, and managing stress. Remember, it's always best to consult with a dermatologist if you're struggling with severe acne.